Abstract
Purpose
To investigate the association between quality of life (QOL) and breakthrough cancer pain (BTCP) intensity in patients who met the commonly accepted definition of BTCP.
Methods
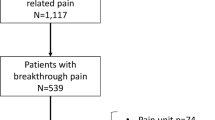
This study was a subset analysis of a South Korean multicenter, non-interventional, cross-sectional, nationwide survey. Participants were recruited from March 2016 to December 2017. BTCP was defined as a controlled background pain of less than a numeric rating scale (NRS) of 3 and any flare-up pain intensity. Pain intensity data were collected using the Brief Pain Inventory (BPI), which includes an interference assessment of the affective and physical domains. Patients were categorized by BTCP intensity into mild (NRS 1–3), moderate (4–6), and severe (7–10) groups.
Results
Of the 969 screened patients with cancer, 679 had ≤ NRS 3 background pain, of whom 438 completed the BPI. Of these 438 patients, 40, 204, and 194 were in the mild, moderate, and severe BTCP groups, respectively. The median NRS of BTCP was 6.0 (interquartile range = 5.0–8.0). Patients with moderate-severe BTCP had significantly higher interference with daily functioning (IDF) scores than did mild BTCP patients (3.3 vs. 5.7; p < 0.01). Both domains of IDF were significantly hampered proportionally by increased BTCP intensity (p < 0.001). The median total IDF scores of the no, moderate, and severe BTCP groups were 3.3, 5.0, and 6.9, respectively. Furthermore, IDF depended on BTCP intensity, duration, and frequency (p < 0.01) but not on pain type and cause.
Conclusion
An increase in BTCP intensity is likely to result in IDF, regardless of the cause or type of BTCP.


Similar content being viewed by others
References
Portenoy RK, Hagen NA (1990) Breakthrough pain: definition, prevalence and characteristics. Pain 41:273–281. https://doi.org/10.1016/0304-3959(90)90004-W
Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G, Science Committee of the Association for Palliative Medicine of Great Britain and Ireland (2008) Breakthrough cancer pain. BMJ 337:a2689. https://doi.org/10.1136/bmj.a2689
Zeppetella G, O’Doherty CA, Collins S (2000) Prevalence and characteristics of breakthrough pain in cancer patients admitted to a hospice. J Pain Symptom Manag 20:87–92. https://doi.org/10.1016/S0885-3924(00)00161-5
Mercadante S, Radbruch L, Caraceni A, Cherny N, Kaasa S, Nauck F, Ripamonti C, De Conno F, Steering Committee of the European Association for Palliative Care (EAPC) Research Network (2002) Episodic (breakthrough) pain: consensus conference of an expert working group of the European Association for Palliative Care. Cancer 94:832–839. https://doi.org/10.1002/cncr.10249
Mercadante S, Marchetti P, Cuomo A, Caraceni A, Mediati RD, Vellucci R, Mammucari M, Natoli S, Lazzari M, Dauri M, Adile C, Airoldi M, Azzarello G, Bandera M, Blasi L, Cartenì G, Chiurazzi B, Costanzo BVP, Degiovanni D, Fusco F, Guardamagna V, Iaffaioli V, Liguori S, Palermo L, Mameli S, Masedu F, Mattioli R, Mazzei T, Melotti RM, Menardo V, Miotti D, Moroso S, Pascoletti G, De Santis S, Orsetti R, Papa A, Ricci S, Scelzi E, Sofia M, Tonini G, Valle A, Aielli F, IOPS-MS Study Group (2018) Factors influencing the clinical presentation of breakthrough pain in cancer patients. Cancers 10:175. https://doi.org/10.3390/cancers10060175
Deandrea S, Corli O, Consonni D, Villani W, Greco MT, Apolone G (2014) Prevalence of breakthrough cancer pain: a systematic review and a pooled analysis of published literature. J Pain Symptom Manag 47:57–76. https://doi.org/10.1016/j.jpainsymman.2013.02.015
Davies AN, Dickman A, Reid C, Stevens AM, Zeppetella G, Science Committee of the Association for Palliative Medicine of Great Britain and Ireland (2009) The management of cancer-related breakthrough pain: recommendations of a task group of the Science Committee of the Association for Palliative Medicine of Great Britain and Ireland. Eur J Pain 13:331–338. https://doi.org/10.1016/j.ejpain.2008.06.014
Bedard G, Davies A, McDonald R, Hawley P, Buchanan A, Popovic M, Wong E, Chow E (2015) Breakthrough cancer pain: a comparison of surveys with European and Canadian patients. Support Care Cancer 23:791–796. https://doi.org/10.1007/s00520-014-2426-6
Baek SK, Kim DY, Kang SY, Sym SJ, Kim YS, Lee JY (2016) A Korean nationwide survey for breakthrough cancer pain in an inpatient setting. Cancer Res Treat 48:768–774. https://doi.org/10.4143/crt.2015.087
Hjermstad MJ, Kaasa S, Caraceni A, Loge JH, Pedersen T, Haugen DF, Aass N, European Palliative Care Research Collaborative (EPCRC) (2016) Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer. BMJ Support Palliat Care 6:344–352. https://doi.org/10.1136/bmjspcare-2015-000887
Gonella S, Sperlinga R, Sciannameo V, Dimonte V, Campagna S (2019) Characteristics of breakthrough pain and its impact on quality of life in terminally ill cancer patients. Integr Cancer Ther 18:1534735419859095. https://doi.org/10.1177/1534735419859095
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap 23:129–138
Yun YH, Mendoza TR, Heo DS, Yoo T, Heo BY, Park HA, Shin HC, Wang XS, Cleeland CS (2004) Development of a cancer pain assessment tool in Korea: a validation study of a Korean version of the brief pain inventory. Oncology 66:439–444. https://doi.org/10.1159/000079497
Raj SX, Thronaes M, Brunelli C, Hjermstad MJ, Klepstad P, Kaasa S (2014) A cross-sectional study on prevalence of pain and breakthrough pain among an unselected group of outpatients in a tertiary cancer clinic. Support Care Cancer 22:1965–1971. https://doi.org/10.1007/s00520-014-2178-3
Davies A, Dickman A, Farquhar-Smith P, Webber K, Zeppetella J (2017) Letter to the Editor re ‘Characteristics of breakthrough cancer pain and its influence on quality of life in an international cohort of patients with cancer (BMJ Support Palliat Care 2016;6:344-52)’. BMJ Support Palliat Care 7:264. https://doi.org/10.1136/bmjspcare-2016-001249
Koh S, Lee K, Oh S, Kang J, Koo D, Yun S, Chang M, Park J, Lee M, Choi Y, Chang J (2019) Assessment, management, and barriers of breakthrough cancer pain: a nationwide study in Korea. Support Care Cancer 27:1–302 eP064
Davies A, Buchanan A, Zeppetella G, Porta-Sales J, Likar R, Weismayr W, Slama O, Korhonen T, Filbet M, Poulain P, Mystakidou K, Ardavanis A, O’Brien T, Wilkinson P, Caraceni A, Zucco F, Zuurmond W, Andersen S, Damkier A, Vejlgaard T, Nauck F, Radbruch L, Sjolund KF, Stenberg M (2013) Breakthrough cancer pain: an observational study of 1000 European oncology patients. J Pain Symptom Manag 46:619–628. https://doi.org/10.1016/j.jpainsymman.2012.12.009
Caraceni A, Martini C, Zecca E, Portenoy RK, Ashby MA, Hawson G, Jackson KA, Lickiss N, Muirden N, Pisasale M, Moulin D, Schulz VN, Rico Pazo MA, Serrano JA, Andersen H, Henriksen HT, Mejholm I, Sjogren P, Heiskanen T, Kalso E, Pere P, Poyhia R, Vuorinen E, Tigerstedt I, Ruismaki P, Bertolino M, Larue F, Ranchere JY, Hege-Scheuing G, Bowdler I, Helbing F, Kostner E, Radbruch L, Kastrinaki K, Shah S, Vijayaram S, Sharma KS, Devi PS, Jain PN, Ramamani PV, Beny A, Brunelli C, Maltoni M, Mercadante S, Plancarte R, Schug S, Engstrand P, Ovalle AF, Wang X, Alves MF, Abrunhosa MR, Sun WZ, Zhang L, Gazizov A, Vaisman M, Rudoy S, Gomez Sancho M, Vila P, Trelis J, Chaudakshetrin P, Koh ML, Van Dongen RT, Vielvoye-Kerkmeer A, Boswell MV, Elliott T, Hargus E, Lutz L, Working Group of an IASP Task Force on Cancer Pain (2004) Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med 18:177–183. https://doi.org/10.1191/0269216304pm890oa
Castel LD, Abernethy AP, Li Y, Depuy V, Saville BR, Hartmann KE (2007) Hazards for pain severity and pain interference with daily living, with exploration of brief pain inventory cutpoints, among women with metastatic breast cancer. J Pain Symptom Manag 34:380–392. https://doi.org/10.1016/j.jpainsymman.2006.12.007
Portenoy RK, Payne D, Jacobsen P (1999) Breakthrough pain: characteristics and impact in patients with cancer pain. Pain 81:129–134. https://doi.org/10.1016/S0304-3959(99)00006-8
Portenoy RK, Bruns D, Shoemaker B, Shoemaker SA (2010) Breakthrough pain in community-dwelling patients with cancer pain and noncancer pain, part 1: prevalence and characteristics. J Opioid Manag 6:97–108. https://doi.org/10.5055/jom.2010.0009
Guitart J, Vargas MI, De Sanctis V, Folch J, Salazar R, Fuentes J, Coma J, Ferreras J, Moya J, Tomás A, Estivill P, Rodelas F, Jiménez AJ (2015) Sublingual fentanyl tablets for relief of breakthrough pain in cancer patients and association with quality-of-life outcomes. Clin Drug Investig 35:815–822. https://doi.org/10.1007/s40261-015-0344-0
Funding
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (1720150) and TEVA Korea. The research was supported by the Korean Cancer Study Group (KCSG) and the KCSG data center.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conceptualization, formal analysis, investigation, original draft preparation, significant data collection, writing, reviewing, and editing. The original draft was prepared and resources provided by Jung Hun Kang and Kyung-Hee Lee. Funding was acquired by Kyung-Hee Lee. All authors read and commented on previous versions of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the 33 institutional review boards and a national research committee (KCSG Protocol Review Committee) as well as with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, J.H., Koh, SJ., Oh, S.Y. et al. Interference with daily functioning by breakthrough pain in patients with cancer. Support Care Cancer 28, 5177–5183 (2020). https://doi.org/10.1007/s00520-020-05329-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05329-9