Abstract
Purpose
This study aims to investigate the impact of possible predictors of quality of life (QoL) in a group of Italian caregivers assisting a cancer patient in home palliative care.
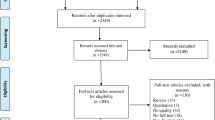
Methods
Data from 570 adult informal caregivers and their cancer-affected relatives were collected. A multivariate regression analysis was conducted to assess the effect of three groups of variables on Caregivers Quality of Life Index-Cancer (CQOLC) scale: (a) socio-demographic characteristics of caregivers; (b) psychological characteristics of caregivers assessed by Profile Mood of States (POMS), Caregiver Burden Inventory (CBI), and Preparedness for Caregiving Scale (PCS); (c) Socio-demographic characteristics and functional status of the patients assessed by Karnofsky Performance Status (KPS), Activities of Daily Living (ADL), and Instrumental Activities of Daily Living (IADL).
Results
Regression analysis shows that some variables from each of these clusters are significantly associated with CQOLC, in particular: (a) the gender of the caregiver (st.β = .115, t = 2.765, p = .006) and the time spent for caregiving (st.β = − .165, t = − 3.960, p < .001); (b) the scores obtained by the caregivers in POMS,CBI (st.β = − .523, t = − 16.984, p < .001 and st.β = − .373, t = − 12.950, p < .001, respectively) and PCS (st.β = .092, t = 3.672, p < .001); (c) the gender (st.β = − .081, t = − 1.933, p = .045) and the IADL score (st.β = .195, t = 4.643, p < .001) of the patient.
Conclusions
A multidimensional evaluation is a key strategy to identify the most vulnerable caregivers. Apart from the condition of the patient, the gender of the caregivers, the time spent for caregiving and, above all, their psychological condition are strong predictors of caregivers’ QoL.
Similar content being viewed by others
References
Vaupel JW (2010) Biodemography of human ageing. Nature 464:536–542. https://doi.org/10.1161/ATVBAHA.114.303112.ApoA-I
European Statistical Office (eurostat) (2016) First population estimates EU population up to slightly over 510 million at 1 January 2016 despite a first ever negative natural change. In: Eurostat Newsrelease http://ec.europa.eu/eurostat/documents/2995521/7553787/3-08072016-AP-EN.pdf/
Colombo F, Llena-Nozal A, Mercier J, Tiadens F (2011) Help wanted? Providing and paying need for long-term care. OECD Heal Policy Stud OECD Publ
Hoffmann F, Rodrigues R (2010) Informal carers: who take care of them? Policy Br April 2010, Eur Cent Soc Welf Policy Res
Istituto Nazionale di Statistica (ISTAT) (2017) Condizioni di salute e ricorso ai servizi sanitari in Italia e nell’Unione europea - Indagine Ehis 2015. https://www.istat.it/it/archivio/204655
Rossi PG, Beccaro M, Miccinesi G et al (2007) Dying of cancer in Italy: impact on family and caregiver. The Italian survey of dying of cancer. J Epidemiol Community Health 61:547–554. https://doi.org/10.1136/jech.2005.045138
Burns CM, Abernethy AP, Dal Grande E, Currow DC (2013) Uncovering an invisible network of direct caregivers at the end of life: a population study. Palliat Med 27:608–615. https://doi.org/10.1177/0269216313483664
Given BA, Given CW, Sherwood PR (2012) Family and caregiver needs over the course of the cancer trajectory. J Support Oncol 10:57–64. https://doi.org/10.1016/j.suponc.2011.10.003
Kent EE, Rowland JH, Northouse L, Litzelman K, Chou WY, Shelburne N, Timura C, O'Mara A, Huss K (2016) Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer 122:1987–1995. https://doi.org/10.1002/cncr.29939
Weitzner MA, McMillan SC, Jacobsen PB (1999) Family caregiver quality of life: differences between curative and palliative cancer treatment settings. J Pain Symptom Manag 17:418–428
Hodgkinson K, Butow P, Hobbs K, Wain G (2007) After cancer: the unmet supportive care needs of survivors and their partners. J Psychosoc Oncol 25:89–104. https://doi.org/10.1300/J077v25n04
Kim Y, Given BA (2008) Quality of life of family caregivers of cancer survivors. Cancer 112:2556–2568. https://doi.org/10.1002/cncr.23449
Milberg A, Wahlberg R, Jakobsson M et al (2011) What is a “secure base” when death is approaching? A study applying attachment theory to adult patients’ and family members’ experiences of palliative home care. Psychooncology 21:886–895. https://doi.org/10.1002/pon.1982
Kitrungrote L, Cohen MZ (2006) Quality of life of family caregivers of patients with cancer: a literature review. Oncol Nurs Forum 33:625–632. https://doi.org/10.1188/06.ONF.625-632
Lapid M, Atherton P, Kung S, Sloan JA, Shahi V, Clark MM, Rummans TA (2015) Cancer caregiver quality of life: need for targeted intervention. Psychooncology 25:1400–1407. https://doi.org/10.1002/pon.3960
Kehoe LA, Xu H, Duberstein P, Loh KP, Culakova E, Canin B, Hurria A, Dale W, Wells M, Gilmore N, Kleckner AS, Lund J, Kamen C, Flannery M, Hoerger M, Hopkins JO, Liu JJ, Geer J, Epstein R, Mohile SG (2019) Quality of life of caregivers of older patients with advanced cancer. J Am Geriatr Soc 67:969–977. https://doi.org/10.1111/jgs.15862
Weitzner MA, Jacobsen PB, Wagner H Jr et al (1999) The Caregiver Quality of Life Index–Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res 8:55–63. https://doi.org/10.1023/a:1026407010614
Nyenhuis DL, Yamamoto C, Lucheta T et al (1999) Adult and geriatric normative data and validation of the profile of mood states. J Clin Psychol 55:79–86. https://doi.org/10.1002/(SICI)1097-4679(199901)55:1<79::AID-JCLP8>3.0.CO;2-7
Novak M, Guest C (1989) Application of a multidimensional caregiver burden inventory. Gerontologist 29:798–803
Henriksson A, Andershed B, Benzein E, Årestedt K (2012) Adaptation and psychometric evaluation of the Preparedness for Caregiving Scale, Caregiver Competence Scale and Rewards of Caregiving Scale in a sample of Swedish family members of patients with life-threatening illness. Palliat Med 26:930–938. https://doi.org/10.1177/0269216311419987
Wade D, Collin C (1988) The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud 10:64–67
Lawton M, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9:179–186
Schag CC, Heinrich RL, Ganz PA (1984) Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol 2:187–193. https://doi.org/10.1200/JCO.1984.2.3.187
Lutzky S, Knight B (1994) Explaining gender differences in caregiver distress: the roles of emotional attentiveness and coping styles. Psychol Aging 9:513–519
Kim Y, Baker F, Spillers RL (2007) Cancer caregivers’ quality of life: effects of gender, relationship, and appraisal. J Pain Symptom Manag 34:294–304. https://doi.org/10.1016/j.jpainsymman.2006.11.012
Garlo K, O’Leary JR, Van Ness PH, Fried TR (2010) Burden in caregivers of older adults with advanced illness. J Am Geriatr Soc 58:2315–2322. https://doi.org/10.1111/j.1532-5415.2010.03177.x
Schrank B, Ebert-Vogel A, Amering M et al (2015) Gender differences in caregiver burden and its determinants in family members of terminally ill cancer patients. Psychooncology 25:808–814. https://doi.org/10.1002/pon.4005
Navaie-Waliser M, Spriggs A, Feldman PH (2002) Informal caregiving: differential experiences by gender. Med Care 40:1249–1259. https://doi.org/10.1097/01.MLR.0000036408.76220.1F
Hagedoorn M, Sanderman R, Ranchor AV, Brilman EI, Kempen GI, Ormel J (2001) Chronic disease in elderly couples: are women more responsive to their spouses’ health condition than men? J Psychosom Res 51:693–696. https://doi.org/10.1016/S0022-3999(01)00279-3
Brazil K, Thabane L, Foster G, Bédard M (2009) Gender differences among Canadian spousal caregivers at the end of life. Heal Soc Care Community 17:159–166. https://doi.org/10.1111/j.1365-2524.2008.00813.x
Baanders AN, Heijmans MJWM (2007) The impact of chronic diseases. The partner ’s perspective. Fam Community Health 30:305–317
Ge L, Mordiffi SZ (2017) Factors associated with higher caregiver burden among family caregivers of elderly cancer patients: a systematic review. Cancer Nurs 40:471–478. https://doi.org/10.1097/NCC.0000000000000445
Iconomou G, Viha A, Kalofonos HP, Kardamakis D (2001) Impact of cancer on primary caregivers of patients receiving radiation therapy. Acta Oncol (Madr) 40:766–771. https://doi.org/10.1080/02841860152619205
Schumacher K, Stewart B, Archbold P (2007) Mutuality and preparedness moderate the effects of caregiving demand on cancer family caregiver outcomes. Nurs Res 56:425–433
Hughes SL, Giobbie-Hurder A, Weaver FM, Kubal JD, Henderson W (1999) Relationship between caregiver burden and health-related quality of life. Gerontologist 39:534–545. https://doi.org/10.1093/geront/39.5.534
Grov EK, Valeberg BT (2012) Does the cancer patient’s disease stage matter? A comparative study of caregivers’ mental health and health related quality of life. Palliat Support Care 10:189–196. https://doi.org/10.1017/S1478951511000873
Weitzner MA, McMillan SC, Jacobsen PB (1999) Family caregiver quality of life. J Pain Symptom Manag 17:418–428. https://doi.org/10.1016/s0885-3924(99)00014-7
Given B (2015) Cargiver Burden. In: Holland J, Weisel T, Nelson C et al (eds) Geriatric psycho-oncology: a quick reference on the psychosocial dimensions of cancer symptom management. Oxford University Press, New York, pp 131–140
Spector WD, Katz S, Murphy JB, Fulton JP (1987) The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis 40:481–489. https://doi.org/10.1016/0021-9681(87)90004-X
Thomas VS, Rockwood K, McDowell I (1998) Multidimensionality in instrumental and basic activities of daily living. J Clin Epidemiol 51:315–321
Ng T, Niti M, Chiam P, Kua E (2006) Physical and cognitive domains of the instrumental activities of daily living: validation in a multiethnic population of Asian older adults. J Gerontol 61A:726–735
Marriott A, Donaldson C, Tarrier N, Burns A (2000) Effectiveness of cognitive–behavioural family intervention in reducing the burden of care in carers of patients with Alzheimer’s disease. Br J Psychiatry 176:557–562. https://doi.org/10.1192/bjp.176.6.557
George C (2016) Valuing the caregiver: an acceptance and commitment therapy group intervention for dementia carers. In: British Psychological Society Annual Conference, Nottingham
Li R, Cooper C, Bradley J, Shulman A, Livingston G (2012) Coping strategies and psychological morbidity in family carers of people with dementia: a systematic review and meta-analysis. J Affect Disord 139:1–11. https://doi.org/10.1016/j.jad.2011.05.055
Yalom I, Leszcz M (2005) The theory and practice of group psychotherapy. Basic Books, New York
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The trial was carried out in full accordance with the Declaration of Helsinki and the Good Clinical Practice. The investigation was approved by the Ethical Committee of the Central Area of Emilia Romagna (AVEC; CE 17001) where the ANT Research Coordination Office is located. Participants provided the informed written consent for participation to the investigation, data analysis, and publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 777 kb)
Rights and permissions
About this article
Cite this article
Franchini, L., Ercolani, G., Ostan, R. et al. Caregivers in home palliative care: gender, psychological aspects, and patient’s functional status as main predictors for their quality of life. Support Care Cancer 28, 3227–3235 (2020). https://doi.org/10.1007/s00520-019-05155-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05155-8