Abstract
Purpose
Adjuvant chemotherapy in patients with breast cancer often causes hot flashes, impairing quality of life. However, the chronobiological or psychiatric factors associated with the development of chemotherapy-induced hot flashes (CIHFs) remain undetermined. The purpose of this study was to investigate whether chronotype was associated with the incidence of CIHFs.
Methods
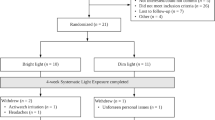
A total of 119 premenopausal women with non-metastatic breast cancer awaiting adjuvant chemotherapy after surgery without hot flashes were included. The presence of CIHF was defined as having moderate to severe hot flashes, as measured by the subscale of hot flashes in the Menopause Rating Scale, at 4 weeks after the completion of chemotherapy. Chronotype (Morning/Intermediate/Evening) was assessed with the Composite Scale of Morningness before adjuvant chemotherapy. To examine the association between chronotype and CIHF, we built logistic regression models, adjusting for age, body mass index, sleep quality, and radiation therapy.
Results
CIHF occurred in 50.4% of participants. Morning type was inversely associated with CIHF (reference: Intermediate type, odds ratio [OR], 0.37; 95% confidence interval [CI], 0.16–0.94; p = 0.040) in the univariate model, and the association remained significant (OR, 0.37; CI, 0.13–0.96; p = 0.045) after adjusting for age, body mass index, sleep quality, and radiation therapy.
Conclusions
Morning chronotype is a protective factor against the development of CIHF in patients with breast cancer. Chronotypes should be assessed and considered in the prediction and management of CIHF.

Similar content being viewed by others
References
Jung K-W, Won Y-J, Kong H-J, Lee ES (2018) Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat 50(2):303–316
Crandall C, Petersen L, Ganz PA, Greendale GA (2004) Association of breast cancer and its therapy with menopause-related symptoms. Menopause 11(5):519–530
Stein KD, Jacobsen PB, Hann DM, Greenberg H, Lyman G (2000) Impact of hot flashes on quality of life among postmenopausal women being treated for breast cancer. J Pain Symptom Manag 19(6):436–445
Carpenter JS, Johnson D, Wagner L, Andrykowski M (2002) Hot flashes and related outcomes in breast cancer survivors and matched comparison women. Oncol Nurs Forum 29(3):E16–E25
Savard J, Liu L, Natarajan L, Rissling MB, Neikrug AB, He F, Dimsdale JE, Mills PJ, Parker BA, Sadler GR, Ancoli-Israel S (2009) Breast cancer patients have progressively impaired sleep-wake activity rhythms during chemotherapy. Sleep 32(9):1155–1160
Savard MH, Savard J, Quesnel C, Ivers H (2009) The influence of breast cancer treatment on the occurrence of hot flashes. J Pain Symptom Manag 37(4):687–697
Lee KM, Jung D, Hwang H et al (2017) Late chronotypes are associated with neoadjuvant chemotherapy-induced nausea and vomiting in women with breast cancer. Chronobiol Int 30(4):480–491
Jung D, Lee KM, Kim WH, Lee JY, Kim TY, Im SA, Lee KH, Spiegel D, Hahm BJ (2016) Longitudinal association of poor sleep quality with chemotherapy-induced nausea and vomiting in patients with breast cancer. Psychosom Med 78:959–965
Lee KM, Jung D, Hwang H, Son KL, Kim TY, Im SA, Lee KH, Hahm BJ (2018) Pre-treatment anxiety is associated with persistent chemotherapy-induced peripheral neuropathy in women treated with neoadjuvant chemotherapy for breast cancer. J Psychosom Res 108:14–19
Carpenter JS, Gilchrist JM, Chen K, Gautam S, Freedman RR (2004) Hot flashes, core body temperature, and metabolic parameters in breast cancer survivors. Menopause 11(4):375–381
Foster RG, Peirson SN, Wulff K, Winnebeck E, Vetter C, Roenneberg T (2013) Sleep and circadian rhythm disruption in social jetlag and mental illness. Prog Mol Biol Transl Sci 119:325–346
Horne JA, Ostberg O (1976) A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol 4(2):97–110
Wittmann M, Dinich J, Merrow M, Roenneberg T (2006) Social jetlag: misalignment of biological and social time. Chronobiol Int 23(1–2):497–509
Heinemann LA, Potthoff P, Schneider HP (2003) International versions of the Menopause Rating Scale (MRS). Health Qual Life Outcomes 1(1):28
National Institutes of Health (2005) National Institutes of Health State-of-the-Science Conference statement: management of menopause-related symptoms. Ann Intern Med 142(12):1003–1013
Barnabei VM, Cochrane BB, Aragaki AK, Nygaard I, Williams RS, McGovern PG, Young RL, Wells EC, O’Sullivan MJ, Chen B, Schenken R, Johnson SR, Women’s Health Initiative I (2005) Menopausal symptoms and treatment-related effects of estrogen and progestin in the Women’s Health Initiative. Obstet Gynecol 105(5 Pt 1):1063–1073, 2005
Sloan JA, Loprinzi CL, Novotny PJ, Barton DL, Lavasseur BI, Windschitl H (2001) Methodologic lessons learned from hot flash studies. J Clin Oncol 19(23):4280–4290
Smith CS, Reilly C, Midkiff K (1989) Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. J Appl Psychol 74(5):728–738
Torsvall L, Åkerstedt T (1980) A diurnal type scale: construction, consistency and validation in shift work. Scand J Work Environ Health 6:283–290
Bohle P, Tilley AJ, Brown S (2001) Psychometric evaluation of the early/late preferences scale. Ergonomics 44(10):887–900
Di Milia L, Adan A, Natale V, Randler C (2013) Reviewing the psychometric properties of contemporary circadian typology measures. Chronobiol Int 30(10):1261–1271
Buysse DJ, Reynolds CF, Monk TH (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Carpenter JS, Andrykowski MA (1998) Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res 45(1):5–13
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67:361–370
Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res 52(2):69–77
Carpenter JS, Gautam S, Freedman RR, Andrykowski M (2001) Circadian rhythm of objectively recorded hot flashes in postmenopausal breast cancer survivors. Menopause 8(3):181–188
Freedman RR (2001) Physiology of hot flashes. Am J Hum Biol 13(4):453–464
Kronenberg F (1990) Hot flashes: epidemiology and physiologya. Ann N Y Acad Sci 592(1):52–86
Negriff S, Dorn LD (2009) Morningness/Eveningness and menstrual symptoms in adolescent females. J Psychosom Res 67(2):169–172
Takeuchi H, Oishi T, Harada T (2005) Association between moringness-eveningness preference and mental/physical premenstrual symptoms in Japanese females 12 to 31 years of age. Chronobiol Int 22(6):1055–1068
Toffol E, Merikanto I, Lahti T, Luoto R, Heikinheimo O, Partonen T (2013) Evidence for a relationship between chronotype and reproductive function in women. Chronobiol Int 30(6):756–765
Funding
This work was supported by the National Research Foundation of Korea (NRF; grant number NRF-2013R1A1A2013480).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. H-1105-092-363), and the clinical trial registration number was NCT 01887925 (WWW.CLINICALTRIALS.GOV).
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. H-1105-092-363).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Son, KL., Jung, D., Lee, KM. et al. Morning chronotype is a protective factor against chemotherapy-induced hot flashes in premenopausal women with breast cancer. Support Care Cancer 28, 1351–1358 (2020). https://doi.org/10.1007/s00520-019-04949-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-04949-0