Abstract
Purpose
Acute leukemia (AL) is associated with substantial morbidity and mortality. We assessed the prevalence and correlates of pain in patients with newly diagnosed or relapsed AL.
Methods
Patients with newly diagnosed or relapsed AL admitted to a comprehensive cancer center completed the Memorial Symptom Assessment Scale (MSAS), which assesses prevalence, severity, and distress associated with pain and other symptoms. Factors associated with severe pain were assessed using logistic regression. Two raters completed chart reviews in duplicate for patients with severe pain (MSAS severity ≥ 3/4) to determine the site of pain.
Results
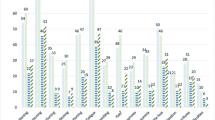
Three hundred eighteen patients were recruited from January 2008 to October 2013: 245 (77.0%) had acute myeloid or acute promyelocytic leukemia (AML/APL) and 73 (23.0%) had acute lymphoblastic leukemia (ALL); 289 (90.9%) were newly diagnosed and 29 (9.1%) had relapsed disease. Pain was reported in 156/318 (49.2%), of whom 55/156 (35.3%) reported severe pain (≥ 3/4). Pain was associated with all psychological symptoms (all p < 0.005) and some physical symptoms. Severe pain was associated with younger age (p = 0.02), worse performance status (p = 0.04), ALL diagnosis (p = 0.04), and time from onset of chemotherapy (p = 0.03), with pain peaking at 4 weeks after chemotherapy initiation. The most common sites of severe pain were oropharynx (22; 40%), head (12; 21.8%), and abdomen (11; 20%). Only 3 patients (0.9%) were referred to the symptom control/palliative care team during the month prior to or following assessment.
Conclusions
Pain is frequent, distressing, and predictable in patients undergoing induction chemotherapy for AL. Further research is needed to assess the efficacy of early supportive care in this population.


Similar content being viewed by others
References
Döhner H, Weisdorf DJ, Bloomfield CD (2015) Acute myeloid leukemia. N Engl J Med 373:1136–1152. https://doi.org/10.1056/NEJMra1406184
Tallman MS, Altman JK (2009) How I treat acute promyelocytic leukemia. Blood 114:5126–5135. https://doi.org/10.1182/blood-2009-07-216457
Terwilliger T, Abdul-Hay M (2017) Acute lymphoblastic leukemia: a comprehensive review and 2017 update. Blood Cancer J 7:e577. https://doi.org/10.1038/bcj.2017.53
Bauduer F, Capdupuy C, Renoux M (2000) Characteristics of deaths in a department of oncohaematology within a general hospital. A study of 81 cases. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 8:302–306
Stalfelt AM, Brodin H, Pettersson S, Eklöf A (2003) The final phase in acute myeloid leukaemia (AML). A study on bleeding, infection and pain. Leuk Res 27:481–488
LeBlanc TW, Smith JM, Currow DC (2015) Symptom burden of haematological malignancies as death approaches in a community palliative care service: a retrospective cohort study of a consecutive case series. Lancet Haematol 2:e334–e338. https://doi.org/10.1016/S2352-3026(15)00111-8
Fadul NA, El Osta B, Dalal S et al (2008) Comparison of symptom burden among patients referred to palliative care with hematologic malignancies versus those with solid tumors. J Palliat Med 11:422–427. https://doi.org/10.1089/jpm.2007.0184
Niscola P, Tendas A, Scaramucci L, Giovaninni M, Cupelli L, de Sanctis V, Brunetti GA, Bondanini F, Palumbo R, Lamanda M, Battistini R, Cartoni C, Romani C, Arcuri E (2011) Pain in malignant hematology. Expert Rev Hematol 4:81–93. https://doi.org/10.1586/ehm.10.79
Zimmermann C, Yuen D, Mischitelle A, Minden MD, Brandwein JM, Schimmer A, Gagliese L, Lo C, Rydall A, Rodin G (2013) Symptom burden and supportive care in patients with acute leukemia. Leuk Res 37:731–736. https://doi.org/10.1016/j.leukres.2013.02.009
Rodin G, Yuen D, Mischitelle A, Minden MD, Brandwein J, Schimmer A, Marmar C, Gagliese L, Lo C, Rydall A, Zimmermann C (2013) Traumatic stress in acute leukemia. Psychooncology 22:299–307. https://doi.org/10.1002/pon.2092
Rodin G, Deckert A, Tong E, Le LW, Rydall A, Schimmer A, Marmar CR, Lo C, Zimmermann C (2018) Traumatic stress in patients with acute leukemia: a prospective cohort study. Psychooncology 27:515–523. https://doi.org/10.1002/pon.4488
Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H (1983) Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry 140:734–739. https://doi.org/10.1176/ajp.140.6.734
Karnofsky DA, Burchenal H (1949) The clinical evaluation of chemotherapeutic agents. In: McCloud CM (ed) Evaluation of chemotherapeutic agents. Columbia University Press, New York, pp 191–205
Rowe JM (2009) Optimal induction and post-remission therapy for AML in first remission. Hematol Am Soc Hematol Educ Program 2009:396–405. https://doi.org/10.1182/asheducation-2009.1.396
Brandwein JM, Gupta V, Schuh AC, Schimmer AD, Yee K, Xu W, Messner HA, Lipton JH, Minden MD (2008) Predictors of response to reinduction chemotherapy for patients with acute myeloid leukemia who do not achieve complete remission with frontline induction chemotherapy. Am J Hematol 83:54–58. https://doi.org/10.1002/ajh.21034
Amadori S, Arcese W, Isacchi G, Meloni G, Petti MC, Monarca B, Testi AM, Mandelli F (1991) Mitoxantrone, etoposide, and intermediate-dose cytarabine: an effective and tolerable regimen for the treatment of refractory acute myeloid leukemia. J Clin Oncol Off J Am Soc Clin Oncol 9:1210–1214. https://doi.org/10.1200/JCO.1991.9.7.1210
Huhmann IM, Watzke HH, Geissler K, Gisslinger H, Jäger U, Knöbl P, Pabinger I, Korninger L, Mannhalter C, Mitterbauer G, Schwarzinger I, Kalhs P, Haas OA, Lechner K (1996) FLAG (fludarabine, cytosine arabinoside, G-CSF) for refractory and relapsed acute myeloid leukemia. Ann Hematol 73:265–271
Portenoy RK, Thaler HT, Kornblith AB, Portenoy RK, Thaler HT, Kornblith AB, Lepore JM, Friedlander-Klar H, Kiyasu E, Sobel K, Coyle N, Kemeny N, Norton L, Scher H (1994) The Memorial Symptom Assessment Scale: an instrument for the evaluation of symptom prevalence, characteristics and distress. Eur J Cancer Oxf Engl 1990(30A):1326–1336
Storring JM, Minden MD, Kao S, Gupta V, Schuh AC, Schimmer AD, Yee KWL, Kamel-Reid S, Chang H, Lipton JH, Messner HA, Xu W, Brandwein JM (2009) Treatment of adults with BCR-ABL negative acute lymphoblastic leukaemia with a modified paediatric regimen. Br J Haematol 146:76–85. https://doi.org/10.1111/j.1365-2141.2009.07712.x
Deshields TL, Potter P, Olsen S, Liu J (2014) The persistence of symptom burden: symptom experience and quality of life of cancer patients across one year. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 22:1089–1096. https://doi.org/10.1007/s00520-013-2049-3
Niscola P (2006) Opioids in pain management of blood-related malignancies. Ann Hematol 85:489–501
Tranmer JE, Heyland D, Dudgeon D, Groll D, Squires-Graham M, Coulson K (2003) Measuring the symptom experience of seriously ill cancer and noncancer hospitalized patients near the end of life with the memorial symptom assessment scale. J Pain Symptom Manage 25:420–429
Cataldo JK, Paul S, Cooper B, Skerman H, Alexander K, Aouizerat B, Blackman V, Merriman J, Dunn L, Ritchie C, Yates P, Miaskowski C (2013) Differences in the symptom experience of older versus younger oncology outpatients: a cross-sectional study. BMC Cancer 13:6. https://doi.org/10.1186/1471-2407-13-6
Posternak V, Dunn LB, Dhruva A, Paul SM, Luce J, Mastick J, Levine JD, Aouizerat BE, Hammer M, Wright F, Miaskowski C (2016) Differences in demographic, clinical, and symptom characteristics and quality of life outcomes among oncology patients with different types of pain. Pain 157:892–900. https://doi.org/10.1097/j.pain.0000000000000456
Cheung WY, Le LW, Gagliese L, Zimmermann C (2011) Age and gender differences in symptom intensity and symptom clusters among patients with metastatic cancer. Support Care Cancer Off J Multinatl Assoc Support Care Cancer 19:417–423. https://doi.org/10.1007/s00520-010-0865-2
Visser MRM, Oort FJ, van Lanschot JJB, van der Velden J, Kloek JJ, Gouma DJ, Schwartz CE, Sprangers MAG (2013) The role of recalibration response shift in explaining bodily pain in cancer patients undergoing invasive surgery: an empirical investigation of the Sprangers and Schwartz model. Psychooncology 22:515–522. https://doi.org/10.1002/pon.2114
Kahn SB, Begg CB, Mazza JJ, Bennett JM, Bonner H, Glick JH (1984) Full dose versus attenuated dose daunorubicin, cytosine arabinoside, and 6-thioguanine in the treatment of acute nonlymphocytic leukemia in the elderly. J Clin Oncol Off J Am Soc Clin Oncol 2:865–870. https://doi.org/10.1200/JCO.1984.2.8.865
Löwenberg B, Ossenkoppele GJ, van Putten W, Schouten HC, Graux C, Ferrant A, Sonneveld P, Maertens J, Jongen-Lavrencic M, von Lilienfeld-Toal M, Biemond BJ, Vellenga E, van Marwijk Kooy M, Verdonck LF, Beck J, Döhner H, Gratwohl A, Pabst T, Verhoef G, Dutch-Belgian Cooperative Trial Group for Hemato-Oncology (HOVON), German AML Study Group (AMLSG), Swiss Group for Clinical Cancer Research (SAKK) Collaborative Group (2009) High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med 361:1235–1248. https://doi.org/10.1056/NEJMoa0901409
Burnett AK, Russell NH, Hills RK, Kell J, Cavenagh J, Kjeldsen L, McMullin M, Cahalin P, Dennis M, Friis L, Thomas IF, Milligan D, Clark RE, UK NCRI AML Study Group (2015) A randomized comparison of daunorubicin 90 mg/m2 vs 60 mg/m2 in AML induction: results from the UK NCRI AML17 trial in 1206 patients. Blood 125:3878–3885. https://doi.org/10.1182/blood-2015-01-623447
Portugal R, Lyrio R, Loureiro M, Urago K, Bard J, Borchardt A, Garnica M, Nucci M (2017) Daunorubicin 90 mg/m2 in acute myeloid leukemia induction: increased toxicity in young patients. Clin Lymphoma Myeloma Leuk 17:527–531. https://doi.org/10.1016/j.clml.2017.06.018
Sonis ST, Sonis AL, Lieberman A (1978) Oral complications in patients receiving treatment for malignancies other than of the head and neck. J Am Dent Assoc 1939(97):468–472
Hui D, Didwaniya N, Vidal M, Shin SH, Chisholm G, Roquemore J, Bruera E (2014) Quality of end-of-life care in patients with hematologic malignancies: a retrospective cohort study. Cancer 120:1572–1578. https://doi.org/10.1002/cncr.28614
Howell DA, Shellens R, Roman E, Garry AC, Patmore R, Howard MR (2011) Haematological malignancy: are patients appropriately referred for specialist palliative and hospice care? A systematic review and meta-analysis of published data. Palliat Med 25:630–641. https://doi.org/10.1177/0269216310391692
Odejide OO, Salas Coronado DY, Watts CD, Wright AA, Abel GA (2014) End-of-life care for blood cancers: a series of focus groups with hematologic oncologists. J Oncol Pract 10:e396–e403. https://doi.org/10.1200/JOP.2014.001537
Hui D, Bansal S, Park M, Reddy A, Cortes J, Fossella F, Bruera E (2015) Differences in attitudes and beliefs toward end-of-life care between hematologic and solid tumor oncology specialists. Ann Oncol Off J Eur Soc Med Oncol 26:1440–1446. https://doi.org/10.1093/annonc/mdv028
LeBlanc TW, O’Donnell JD, Crowley-Matoka M, Rabow MW, Smith CB, White DB, Tiver GA, Arnold RM, Schenker Y (2015) Perceptions of palliative care among hematologic malignancy specialists: a mixed-methods study. J Oncol Pract 11:e230–e238. https://doi.org/10.1200/JOP.2014.001859
El-Jawahri A, LeBlanc T, VanDusen H, Traeger L, Greer JA, Pirl WF, Jackson VA, Telles J, Rhodes A, Spitzer TR, McAfee S, Chen YA, Lee SS, Temel JS (2016) Effect of inpatient palliative care on quality of life 2 weeks after hematopoietic stem cell transplantation: a randomized clinical trial. JAMA 316:2094–2103. https://doi.org/10.1001/jama.2016.16786
Zimmermann C (2016) Palliative care for patients with hematological malignancies: time for a new model. Leuk Res 48:78–79. https://doi.org/10.1016/j.leukres.2016.07.012
LeBlanc TW (2014) Palliative care and hematologic malignancies: old dog, new tricks? J Oncol Pract 10:e404–e407. https://doi.org/10.1200/JOP.2014.000968
Othus M, Kantarjian H, Petersdorf S, Ravandi F, Godwin J, Cortes J, Pierce S, Erba H, Faderl S, Appelbaum FR, Estey E (2014) Declining rates of treatment-related mortality in patients with newly diagnosed AML given “intense” induction regimens: a report from SWOG and MD Anderson. Leukemia 28:289–292. https://doi.org/10.1038/leu.2013.176
Acknowledgments
The authors would like to thank our clinical and research staff who contributed to this project, and especially the study participants who gave their time and effort to help us better understand the experience of living with acute leukemia.
Funding
Funding for this study was provided by the Canadian Institutes of Health Research (#MOP 84317; GR and CZ, Co-Principal Investigators); the present analysis and write-up were supported in part by the Canadian Cancer Society (grant #702603; GR and CZ, Co-PIs). The research was also supported in part by the Princess Margaret Cancer Centre and Princess Margaret Cancer Foundation, University Health Network, Toronto, Canada, and by the Ministry of Health and Long-term Care. GR holds the University of Toronto/University Health Network Harold and Shirley Lederman Chair in Psychosocial Oncology and Palliative Care; and CZ holds the Rose Family Chair in Palliative Medicine and Supportive Care from the University of Toronto. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
Conception and design: AS, CZ, GR.
Administrative support: AR.
Provision of study materials or patients: ADS.
Study implementation, acquisition and/or assembly of data: AS, GP, VBC, AR.
Analysis and interpretation of data: LWL, AS, ADS, CZ, GR.
Manuscript writing: All authors.
Final approval of manuscript to be published: All authors.
Corresponding author
Ethics declarations
This study received approval from the University Health Network (UHN) Research Ethics Board (REB #06-0387-CE). All study participants provided written informed consent.
Conflict of interest
A.D. Schimmer reports personal fees and grants outside this submitted work from Novartis, Takeda Pharmaceuticals, Aeglea Pharmaceuticals, and Trillium Therapeutics. The remaining authors declare no conflicts of interest.
Prior presentation
Findings were presented in part at the Multinational Association of Supportive Care in Cancer (MASCC)/ISOO 2017 Annual Meeting on Supportive Care in Cancer, Washington, DC, USA, June 22–24, 2017 (e-poster presentation); early/preliminary findings were presented at the 20th International Congress on Palliative Care, Montreal, Quebec, Canada, September 9–12, 2014 (poster presentation); the MASCC/ISOO 2014 Annual Meeting on Supportive Care in Cancer, Miami, Florida, United States, June 26–28, 2014 (oral presentation); the Hospice Palliative Care Ontario Annual Conference, Toronto, Ontario, Canada, April 27–29, 2014 (oral presentation); and the 9th Annual Advanced Learning in Palliative Medicine Conference, Vancouver, British Columbia, Canada, June 13–15, 2013 (oral presentation).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shaulov, A., Rodin, G., Popovic, G. et al. Pain in patients with newly diagnosed or relapsed acute leukemia. Support Care Cancer 27, 2789–2797 (2019). https://doi.org/10.1007/s00520-018-4583-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4583-5