Abstract
Purpose
To assess sexual health and needs for sexology care of cancer patients during chemotherapy.
Methods
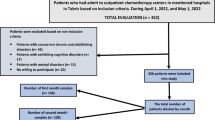
We performed a 4-month cross-sectional study in cancer patients treated by chemotherapy in the digestive cancer department of a regional university hospital. Patients were asked to fill out a self-administered questionnaire about their sexual health, Sexual Quality of Life Questionnaire for Male (SQoL-M) or Female (SQoL-F), and their needs for sexology care.
Results
The study sample was composed of 47 men and 31 women. Tumor locations were 36 colorectal (46%), 23 pancreatic (30%), and 19 other digestive cancers (24%). SQoL scores were lower in women (p < .001), in pancreatic and colorectal tumors (p = .041 and p = .033, respectively) compared to other digestive cancers, and in less-educated patients (p = .023). During chemotherapy, 40% of sexually active patients had less frequent sexual intercourse than before diagnosis, and 33% had completely stopped sexual activity. Sexuality care was desired by 44% of respondents. Among them, 83% favored a consultation with a medical sexologist and 63% with a psycho-sexologist, 54% wanted couple therapy, and 31% considered support groups. Patients with colorectal cancer had more frequent sexual intercourse without penetration at the time of survey (p = .036) and more often wanted couple therapy than patients with pancreatic cancer (p = .048).
Conclusions
This study is the first determination of sexual health and sexual quality of life in digestive cancers. Targets for interventions during chemotherapy for digestive cancers include populations with lower sexual quality of life: women, pancreatic sites, patients with sexual troubles during chemotherapy, and less-educated patients.

Similar content being viewed by others
References
Schover LR, van der Kaaij M, van Dorst E, Creutzberg C, Huyghe E, Kiserud CE (2014) Sexual dysfunction and infertility as late effects of cancer treatment. Eur J Cancer Suppl 12(1):41–53. https://doi.org/10.1016/j.ejcsup.2014.03.004
Sadovsky R, Basson R, Krychman M, Morales AM, Schover L, Wang R, Incrocci L (2010) Cancer and sexual problems. J Sex Med 7(1 Pt 2):349–373. https://doi.org/10.1111/j.1743-6109.2009.01620.x
National Health Institute (2006) The prevalence and types of sexual dysfunction in people with cancer. https://www.cancer.gov. Accessed 13 June 2012
Bober SL, Varela VS (2012) Sexuality in adult cancer survivors: challenges and intervention. J Clin Oncol 30(30):3712–3719. https://doi.org/10.1200/JCO.2012.41.7915
Brotto LA, Yule M, Breckon E (2010) Psychological interventions for the sexual sequelae of cancer: a review of the literature. J Cancer Surviv 4(4):346–360. https://doi.org/10.1007/s11764-010-0132-z
Le Corroller-Soriano AG, Malavolti L, Mermilliod C (2008) La vie deux ans après le diagnostic de cancer, La Documentation Française edn. DRESS, INSERM: Collection Etudes et Statistiques, Paris
Institut National du Cancer (2014) La vie deux ans après un diagnostic de cancer - De l’annonce à l’après cancer. http://www.e-cancer.fr/Expertises-et-publications/Catalogue-des-publications/La-vie-deux-ans-apres-un-diagnostic-de-cancer-De-l-annonce-a-l-apres-cancer
Breukink SO, Donovan KA (2013) Physical and psychological effects of treatment on sexual functioning in colorectal cancer survivors. J Sex Med 10(Suppl 1):74–83. https://doi.org/10.1111/jsm.12037
Daniels IR, Woodward S, Taylor FG, Raja A, Toomey P (2006) Female urogenital dysfunction following total mesorectal excision for rectal cancer. World J Surg Oncol 4:6. https://doi.org/10.1186/1477-7819-4-6
Cornish JA, Tan E, Teare J, Teoh TG, Rai R, Darzi AW, Paraskevas P, Clark SK, Tekkis PP (2007) The effect of restorative proctocolectomy on sexual function, urinary function, fertility, pregnancy and delivery: a systematic review. Dis Colon Rectum 50(8):1128–1138. https://doi.org/10.1007/s10350-007-0240-7
Lange MM, Marijnen CA, Maas CP, Putter H, Rutten HJ, Stiggelbout AM, Meershoek-Klein Kranenbarg E, van de Velde CJ, Cooperative clinical investigators of the D (2009) Risk factors for sexual dysfunction after rectal cancer treatment. Eur J Cancer 45(9):1578–1588. https://doi.org/10.1016/j.ejca.2008.12.014
Frick MA, Vachani CC, Hampshire MK, Bach C, Arnold-Korzeniowski K, Metz JM, Hill-Kayser CE (2017) Survivorship after lower gastrointestinal cancer: patient-reported outcomes and planning for care. Cancer 123(10):1860–1868. https://doi.org/10.1002/cncr.30527
Adekanle O, Ndububa DA, Orji EO, Ijarotimi O (2014) Assessment of the sexual functions of males with chronic liver disease in South West Nigeria. Ann Afr Med 13(2):81–86. https://doi.org/10.4103/1596-3519.129884
Kosenow W, Feil G, von Torne H, Bierich JR, Apostolakis M (1967) Early sexual riping caused by primary liver carcinoma: “hepatogenital syndrome”. Monatsschr Kinderheilkd 115(1):37–46
Steel J, Hess SA, Tunke L, Chopra K, Carr BI (2005) Sexual functioning in patients with hepatocellular carcinoma. Cancer 104(10):2234–2243. https://doi.org/10.1002/cncr.21450
Regi P, Salvia R, Cena C, Girelli R, Frigerio I, Bassi C (2013) Cystic “feminine” pancreatic neoplasms in men. Do any clinical alterations correlate with these uncommon entities? Int J Surg 11(2):157–160. https://doi.org/10.1016/j.ijsu.2012.12.008
Habold D, Farsi F (2012) Cancer, santé sexualité et intimité. Référentiel AFSOS. http://www.afsos.org/wp-content/uploads/2016/09/Cancer_vie_et_sante_sexuelle.pdf. Accessed 17 Jan 2017
Chen RC, Clark JA, Talcott JA (2009) Individualizing quality-of-life outcomes reporting: how localized prostate cancer treatments affect patients with different levels of baseline urinary, bowel, and sexual function. J Clin Oncol 27(24):3916–3922. https://doi.org/10.1200/JCO.2008.18.6486
Almont T, Delannes M, Ducassou A, Corman A, Bondil P, Moyal E, Schover L, Eric H (2017) Sexual quality of life and needs for sexual care of cancer patients admitted for radiotherapy: a 3-month cross-sectional study. J Sex Med 14(4):566–576. https://doi.org/10.1016/j.jsxm.2017.02.013
Huyghe E, Sui D, Odensky E, Schover LR (2009) Needs assessment survey to justify establishing a reproductive health clinic at a comprehensive cancer center. J Sex Med 6(1):149–163. https://doi.org/10.1111/j.1743-6109.2008.01005.x
Symonds T, Boolell M, Quirk F (2005) Development of a questionnaire on sexual quality of life in women. J Sex Marital Ther 31(5):385–397. https://doi.org/10.1080/00926230591006502
Abraham L, Symonds T, Morris MF (2008) Psychometric validation of a sexual quality of life questionnaire for use in men with premature ejaculation or erectile dysfunction. J Sex Med 5(3):595–601. https://doi.org/10.1111/j.1743-6109.2007.00749.x
Abraham L, Symonds T, May K, Althof SE, Hallam-Jones R, Rosen RC (2009) Psychometric validation of gender nonspecific sexual confidence and sexual relationship scales in men and women. J Sex Med 6(8):2244–2254. https://doi.org/10.1111/j.1743-6109.2009.01336.x
Letourneau JM, Smith JF, Ebbel EE, Craig A, Katz PP, Cedars MI, Rosen MP (2012) Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer 118(18):4579–4588. https://doi.org/10.1002/cncr.26649
Vitrano V, Catania V, Mercadante S (2011) Sexuality in patients with advanced cancer: a prospective study in a population admitted to an acute pain relief and palliative care unit. Am J Hosp Palliat Care 28(3):198–202. https://doi.org/10.1177/1049909110386044
Mercadante S, Vitrano V, Catania V (2010) Sexual issues in early and late stage cancer: a review. Support Care Cancer 18(6):659–665. https://doi.org/10.1007/s00520-010-0814-0
Lemieux L, Kaiser S, Pereira J, Meadows LM (2004) Sexuality in palliative care: patient perspectives. Palliat Med 18(7):630–637. https://doi.org/10.1191/0269216304pm941oa
Braun DP, Gupta D, Staren ED (2013) Longitudinal health-related quality of life assessment implications for prognosis in stage IV pancreatic cancer. Pancreas 42(2):254–259. https://doi.org/10.1097/MPA.0b013e31825b9f56
Jia L, Shang Y, Jiang S, Xie Q, Huang Y, Xie D, Huang K, Zhi F, Li Y (2009) Relationship between symptoms of pancreatic cancer-related depression and quality of life of patients. Zhonghua Yi Xue Za Zhi 89(26):1847–1849
Pezzilli R, Falconi M, Zerbi A, Casadei R, Valli L, Varale R, Armatura G, Felicani C, Morselli-Labate AM (2011) Clinical and patient-reported outcomes after pancreatoduodenectomy for different diseases: a follow-up study. Pancreas 40(6):938–945. https://doi.org/10.1097/MPA.0b013e318216f693
Shaw CM, O’Hanlon DM, McEntee GP (2005) Long-term quality of life following pancreaticoduodenectomy. Hepato-Gastroenterology 52(63):927–932
Velanovich V (2011) The association of quality-of-life measures with malignancy and survival in patients with pancreatic pathology. Pancreas 40(7):1063–1069. https://doi.org/10.1097/MPA.0b013e31821ad8eb
Anwar S, Tan W, Yu J, Hutson A, Javle M, Iyer R (2014) Quality-of-life (QoL) as a predictive biomarker in patients with advanced pancreatic cancer (APC) receiving chemotherapy: results from a prospective multicenter phase 2 trial. J Gastrointest Oncol 5(6):433–439. https://doi.org/10.3978/j.issn.2078-6891.2014.070
Pezzilli R, Campana D, Morselli-Labate AM, Fabbri MC, Brocchi E, Tomassetti P (2009) Patient-reported outcomes in subjects with neuroendocrine tumors of the pancreas. World J Gastroenterol 15(40):5067–5073
Sun V, Grant M, Wendel CS, McMullen CK, Bulkley JE, Herrinton LJ, Hornbrook MC, Krouse RS (2016) Sexual function and health-related quality of life in long-term rectal cancer survivors. J Sex Med 13(7):1071–1079. https://doi.org/10.1016/j.jsxm.2016.05.005
Kohler TS, Pedro R, Hendlin K, Utz W, Ugarte R, Reddy P, Makhlouf A, Ryndin I, Canales BK, Weiland D, Nakib N, Ramani A, Anderson JK, Monga M (2007) A pilot study on the early use of the vacuum erection device after radical retropubic prostatectomy. BJU Int 100(4):858–862. https://doi.org/10.1111/j.1464-410X.2007.07161.x
Amar E (2005) The interest of early rehabilitation with intracavernous injections following complete prostatectomy. Presse Med 34(13 Suppl):15–18
Melisko ME, Goldman ME, Hwang J, De Luca A, Fang S, Esserman LJ, Chien AJ, Park JW, Rugo HS (2017) Vaginal testosterone cream vs estradiol vaginal ring for vaginal dryness or decreased libido in women receiving aromatase inhibitors for early-stage breast cancer: a randomized clinical trial. JAMA Oncol 3(3):313–319. https://doi.org/10.1001/jamaoncol.2016.3904
Rosenberg SM, Tamimi RM, Gelber S, Ruddy KJ, Bober SL, Kereakoglow S, Borges VF, Come SE, Schapira L, Partridge AH (2014) Treatment-related amenorrhea and sexual functioning in young breast cancer survivors. Cancer 120(15):2264–2271. https://doi.org/10.1002/cncr.28738
Puts MT, Papoutsis A, Springall E, Tourangeau AE (2012) A systematic review of unmet needs of newly diagnosed older cancer patients undergoing active cancer treatment. Support Care Cancer 20(7):1377–1394. https://doi.org/10.1007/s00520-012-1450-7
Hall AE, Boyes AW, Bowman J, Walsh RA, James EL, Girgis A (2012) Young adult cancer survivors’ psychosocial well-being: a cross-sectional study assessing quality of life, unmet needs, and health behaviors. Support Care Cancer: Off J Multinatl Assoc Support Care Cancer 20(6):1333–1341. https://doi.org/10.1007/s00520-011-1221-x
McCallum M, Lefebvre M, Jolicoeur L, Maheu C, Lebel S (2012) Sexual health and gynecological cancer: conceptualizing patient needs and overcoming barriers to seeking and accessing services. J Psychosom Obstet Gynaecol 33(3):135–142. https://doi.org/10.3109/0167482X.2012.709291
Reese JB, Shelby RA, Abernethy AP (2011) Sexual concerns in lung cancer patients: an examination of predictors and moderating effects of age and gender. Support Care Cancer 19(1):161–165. https://doi.org/10.1007/s00520-010-1000-0
Dyer K, das Nair R (2013) Why don’t healthcare professionals talk about sex? A systematic review of recent qualitative studies conducted in the United Kingdom. J Sex Med 10(11):2658–2670. https://doi.org/10.1111/j.1743-6109.2012.02856.x
Park ER, Norris RL, Bober SL (2009) Sexual health communication during cancer care: barriers and recommendations. Cancer J 15(1):74–77. https://doi.org/10.1097/PPO.0b013e31819587dc
Acknowledgments
We gratefully acknowledge Dr. Deslandres Marion and Dr. Anne-Pascale Laurenty for their valuable insights for implementing this study and particularly the oncology teams of the Digestive Cancer Department who helped in the recruitment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Each patient was given a verbal explanation of the study by TA and signed a written informed consent. The study was approved by the French Advisory Committee for Data Processing in Health Research (CCTIRS) under the number 16.037.
Conflict of interest
The study was methodologically supported by the University Cancer Center of Toulouse (University Hospital of Rangueil), the Cancer Network of Midi-Pyrénées (ONCOMIP), the Association of Coordinators of the French Cancer Networks (ACORESCA), the joint group of the Federative Group of French Cancer Centers (UNICANCER) and the French Association for Supportive Care (AFSOS), and the French Education and Research Group of Andrology, Urology, and Sexology (GEFRAUS).
This project was granted by the French National League Against Cancer (PhD grant no. TDTJ12441 — 2013e2016). The authors report having no financial relationship with the organization that sponsored the research. The authors also declare having full control of all primary data and agree to allow the journal to review their data if requested.
Rights and permissions
About this article
Cite this article
Almont, T., Couteau, C., Etienne, H. et al. Sexual health and needs for sexology care in digestive cancer patients undergoing chemotherapy: a 4-month cross-sectional study in a French University Hospital. Support Care Cancer 26, 2889–2899 (2018). https://doi.org/10.1007/s00520-018-4125-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4125-1