Abstract
Background
This study examined which patient- and physician-related factors influence guideline violations in adjuvant chemotherapy.
Patients and methods
In a prospective multi-center cohort study, patients with primary breast cancer were sampled consecutively over a period of four years (2009–2012). Patients completed a questionnaire prior to surgery and prior to adjuvant therapy. This questionnaire assessed health-related quality of life (QoL) using the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30, psychiatric co-morbidity with the Patient Health Questionnaire (PHQ), demographic characteristics (age, education), and the intensity of fear for chemotherapy.
After surgery, a multi-professional team discussed recommendation for adjuvant chemotherapy, and this decision was documented in a database together with the indication for chemotherapy according to the German S3 guideline. This multi-professional team was blinded to that algorithm-based decision. Six months later, it was documented whether the patient had received adjuvant chemotherapy or not.
Results
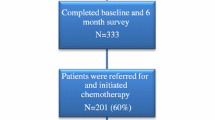
Altogether, 857 patients were included in the study. In 391 of these patients, the tumor board (TB) decided to recommend chemotherapy. The most important reasons for not recommending chemotherapy were somatic co-morbidity not allowing adjuvant chemotherapy and age >75 years.
Of these 391 patients, 73 (19 %) patients eventually did not receive chemotherapy. Deviations from the initial therapy decision were more frequent in older patients (≥75 years) with poor QoL. If the QoL was good, higher age was not related to deviation. There was some evidence that patients with higher education less frequently received chemotherapy (CT). Furthermore, if patients were very afraid of chemotherapy, deviations from the initial therapy decision were more likely. Co-morbidity and fear of CT were not related to the likelihood of deviating from the initial therapy decision.
Conclusion
Nineteen percent of patients eventually did not receive chemotherapy, despite guideline and TB recommendations. In these patients, this mainly occurred in association with poor QoL in elderly patients >75 years old. In the group with a chemotherapy recommendation, patients’ fear of chemotherapy is another factor preventing patients from undergoing adjuvant chemotherapy.

Similar content being viewed by others
References
Robert-Koch-Institute, Breast cancer incidence in Germany 2014, http://www.rki.de/Krebs/DE/Content/Krebsarten/Brustkrebs/brustkrebs_node.html. Accessed 1 Jul 2015.
Van Ewijk R, Schwentner L, Wöckel A, König J, Kreienberg R, Blettner M (2013) Trends in patient characteristics, treatment and survival in breast cancer in a non-selected retrospective clinical cohort study of 2,600 patients. Arch Gynecol Obstet 287(1):103–10
Van Luijt PA, Fracheboud J, Heijnsdijk EA, den Heeten GJ, de Koning HJ, National evaluation team for breast cancer screening in Netherlands study groups (NETB) (2013) Nation-wide data on screening performance during the transition to digital mammography: observations in 6 million screens. Eur J Cancer 49(16):3517–25
Wo JY, Chen K, Neville BA, Lin NU, Punglia RS (2011) Effect of very small tumor size on cancer-specific mortality in node-positive breast cancer. J Clin Oncol 29(19):2619–27
Kowalski C, Ferencz J, Brucker SY, Kreienberg R, Wesselmann S. Quality of care in breast cancer centers: results of benchmarking by the German Cancer Society and German Society for Breast Disease. Breast 2014; doi: 10.1016/j.breast.2014.11.014
Hancke K, Denkinger MD, König J, Kurzeder C, Wöckel A, Herr D et al (2010) Standard treatment of female patients with breast cancer decreases substantially for women aged 70 years and older: a German clinical cohort study. Ann Oncol 21(4):748–53
Schwentner L, Wolters R, Wischnewsky MB, Kreienberg R, Wöckel A (2010) Survival of patients with bilateral versus unilateral breast cancer and impact of guideline adherent adjuvant treatment: a multi-centre cohort study of 5292 patients. Breast 21(2):171–7
Schwentner L, Wolters R, Koretz K, Wischnewsky MB, Kreienberg R, Rottscholl R et al (2012) Triple-negative breast cancer: the impact of guideline-adherent adjuvant treatment on survival—a retrospective multi-centre cohort study. Breast Cancer Res Treat 132(3):1073–80
Wolters R, Wöckel A, Janni W, Novopashenny I, Ebner F, Kreienberg R et al (2013) Comparing the outcome between multicentric and multifocal breast cancer: what is the impact on survival and is there a role for guideline-adherent adjuvant therapy? A retrospective multi-center cohort study of 8,935 patients. Breast Cancer Res Treat 142(3):579–90
Wöckel A, Wolters R, Wiegel T, Novopashenny I, Janni W, Kreienberg R et al (2014) The impact of adjuvant radiotherapy on the survival of primary breast cancer patients: a retrospective multicenter cohort study of 8935 subjects. Ann Oncol 25(3):628–32
Hebert-Croteau N, Brisson J, Latreille J, Rivard M, Abdelaziz N, Martin G (2004) Compliance with consensus recommendations for systemic therapy is associated with improved survival of women with nodal negative breast cancer. J Clin Oncol 22:3685–93
Ziller V, Kyvernitakis I, Knöll D, Storch A, Hars O, Hadji P (2013) Influence of a patient information program on adherence and persistence with an aromatase inhibitor in breast cancer treatment—the COMPAS study. BMC Cancer 13:407
D‘Hoore W, Sicotte C, Tiquin C (1993) Risk adjustment in outcome assessment: the Charlson comorbidity index. Methods Inf Med 32:382–7
Löwe B, Spitzer RL, Zipfel S, Herzog W (2002) PHQ-D Gesundheitsfragebogen für Patienten. Pfizer, Manual. Karlsruhe
Spitzer RL, Williams J, Kroenke K (1999) Prime MD today. Evaluation of metal disorders. Pfizer, New York
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ et al (1993) The European Organization For Research And Treatment Of Cancer QLQ-C30—a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–76
Schwarz R, Hinz A (2001) Reference data for the quality of life questionnaire EORTC QLQ-C30 in the general German population. EurJ Cancer 37:1345–51
Lerman CE, Brody DS, Caputo GC, Smith DG, Lazaro CG, Wolfson HG (1990) Patients’ perceived involvement in care scale: relationship to attitudes about illness and medical care. J Gen Intern Med 5:29–33
Scheibler F, Freise D, Pfaff H (2004) Die Einbeziehung von Patienten in die Behandlung—Validierung der deutschen PICS-Skalen. J Publ Health 12:199–209
Kreienberg R, Kopp I, Albert U, Bartsch H, Beckmann MW, Berg D, et al. Interdisciplinary S3 guideline for diagnosis and therapy of breast cancer in women. German cancer society 2008
Wolters R, Regierer AC, Schwentner L, Geyer V, Possinger K, Kreienberg R et al (2012) A comparison of international breast cancer guidelines—do the national guidelines differ in treatment recommendations? Eur J Cancer 48(1):1–11
Goldhirsch A, Wood WC, Gelber RD, Coates AS, Thürlimann B, Senn HJ (2007) Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol 18(7):1133–44
Neugut AI, Hillyer GC, Kushi LH, Lamerato L, Leoce N, Nathanson SD et al (2012) Noninitiation of adjuvant chemotherapy in women with localized breast cancer: the breast cancer quality of care study. J Clin Oncol 30(31):3800–9
Barron TI, Cahir C, Sharp L, Bennett K (2013) A nested case-control study of adjuvant hormonal therapy persistence and compliance, and early breast cancer recurrence in women with stage I–III breast cancer. Br J Cancer 109:1513–21
Harbeck N, Blettner M, Hadji P, Jakisch C, Lück HJ, Windermuth-Kieselbach C et al (2013) Patient’s Anastrozole Compliance to Therapy (PACT) program: baseline data and patient characteristics from a population-based, randomized study evaluating compliance to aromatase inhibitor therapy in postmenopausal women with hormone-sensitive early breast cancer. Breast Care (Basel) 8(2):110–20
Banning M (2012) Adherence to adjuvant therapy in post-menopausal breast cancer patients: a review. Eur J Cancer Care 21(1):10–9
Schouten LJ, Jager JJ, van den Brandt PA (1993) Quality of cancer registry data: a comparison of data provided by clinicians with those of registrations personnel. Br J Cancer 68(5):974–7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study and the BRENDA project have been approved by the ethics committee of the University of Ulm.
Conflict of interest
The authors declare that they have no competing interests.
Funding source
This work was supported by the German Federal Ministry of Education and Research (BMBF-Grant-01ZP0505).
Rights and permissions
About this article
Cite this article
Schwentner, L., Van Ewijk, R., Kühn, T. et al. Exploring patient- and physician-related factors preventing breast cancer patients from guideline-adherent adjuvant chemotherapy—results from the prospective multi-center study BRENDA II. Support Care Cancer 24, 2759–2766 (2016). https://doi.org/10.1007/s00520-016-3088-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-016-3088-3