Abstract
Purpose
Dexamethasone, plus a 5-HT3 receptor antagonist and an NK-1 receptor antagonist are recommended for controlling the chemotherapy-induced nausea and vomiting (CINV) of highly emetogenic chemotherapy. Several days of dexamethasone are effective for CINV; however, dexamethasone also has side effects. The purpose of this trial was to investigate whether the use of a second-generation 5-HT3 receptor antagonist and an NK-1 receptor antagonist could allow a reduced dose of dexamethasone for breast cancer patients receiving highly emetogenic chemotherapy.
Methods
Eighty breast cancer patients who received an anthracycline-cyclophosphamide combination regimen were enrolled. The patients were randomized to arm A (dexamethasone days 1–3) and arm B (dexamethasone day 1). The primary endpoint was complete response (CR) (no emetic episodes and no rescue medication) during the overall phase (days 1–5). The secondary endpoints were the CR during the delayed phase (days 2–5), complete control (CC) (no emetic episodes, no rescue medication, and no more than mild nausea) during the overall phase, and the safety of this antiemetic therapy.
Results
There were no significant differences in the rates of CR and CC between arm A and B as follows: CR overall phase—arm A: 82.9 %, 90 % confidence interval [CI] 71.3–90.5 % vs arm B: 82.1 %, 90 % CI 70.0–90.0 %; p = 1.00; CR delayed phase—arm A: 87.8 %, 90 % CI 77.0–93.9 % vs arm B: 94.9 %, 90 % CI 85.6–98.3 %; p = 0.43; CC overall phase—arm A: 48.8 %, 90 % CI 36.4–61.3 % vs arm B: 61.5 %, 90 % CI 48.4–73.2 %; p = 0.27. There were very few adverse events and no severe adverse events associated with this antiemetic therapy.
Conclusions
The results suggest that the antiemetic effect provided by dexamethasone administered for 3 days can be obtained by dexamethasone administered for 1 day.
Similar content being viewed by others
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is a major nonhematologic toxicity associated with chemotherapy. CINV not only affects quality of life but also compliance with chemotherapy [1]. CINV varies, depending on the type, dosage, and route of administration of the antineoplastic agent. Chemotherapy regimens have been classified according to the incidence of nausea. A regimen associated with emesis in ≥90 % of patients was considered to have high emetic risk (highly emetogenic chemotherapy [HEC]); with emesis in 30 to 90 % of patients, a moderate emetic risk (moderately emetogenic chemotherapy [MEC]); with emesis in 10 to 30 % of patients, a low emetic risk; and with emesis in fewer than 10 % of patients, a minimal emetic risk [2, 3]. A chemotherapy regimen for breast cancer containing an anthracycline such as doxorubicin and epirubicin in combination with cyclophosphamide is classified as HEC. Based on the antiemesis guidelines of the National Comprehensive Cancer Network (NCCN, www.nccn.org), the American Society for Clinical Oncology (ASCO) [4], and the Multinational Association for Supportive Care in Cancer (MASCC, www.mascc.org), the recommended treatment for preventing CINV associated with HEC is palonosetron, a serotonin (5-HT3) receptor antagonist; aprepitant, a neurokinin 1 (NK-1) antagonist; and dexamethasone.
Palonosetron is a second-generation 5-HT3 receptor antagonist. It has a higher binding affinity to 5-HT3 receptors [5] and a longer elimination half-life than the first-generation antagonists. Palonosetron has been found to provide better control of CINV during the acute and delayed phases than the first-generation 5-HT3 receptor antagonists [6, 7].
Dexamethasone administration is recommended until day 4 of treatment by the NCCN guidelines to prevent delayed phase emesis. However, frequent steroid administration during chemotherapy is associated with problematic side effects such as edema, bulimia, weight gain, digestive disorders, moon face, hyperglycemia, and reactivation of hepatitis B virus [8–10]. Reducing the dose of steroids with resulting reduction in side effects may be beneficial for patients undergoing chemotherapy. To the best of our knowledge, there have not been any reported studies on the use of aprepitant and palonosetron to decrease the dose of dexamethasone. The aim of this study was to evaluate the antiemetic effects of palonosetron and aprepitant combined with 1 day of dexamethasone administration. This was a single-blind, single-center randomized controlled phase II trial of breast cancer patients receiving an anthracycline-cyclophosphamide combination regimen.
Patients and methods
Inclusion criteria
The patients who were eligible for inclusion were chemotherapy-naive female patients with histologically confirmed breast cancer, ≥20 years of age, and scheduled to receive an anthracycline-cyclophosphamide combination regimen. Additional inclusion criteria included Eastern Cooperative Oncology Group (ECOG) performance status 0–1, adequate general condition (white blood cell count 3 × 109 cells/L), hepatic function (aspartate aminotransferase [AST] and alanine aminotransferase [ALT] < 100 U/L), and renal function (creatinine clearance ≥60 mL/min).
Exclusion criteria
Exclusion criteria included seizure disorder needing anticonvulsants, unless clinically stable; any vomiting, retching, or grade 2 or higher nausea according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTCAE); asymptomatic metastases to the brain; known hypersensitivity to palonosetron, aprepitant or dexamethasone ingredients; pregnancy/breast-feeding; receiving any drug with antiemetic effects; and receiving pimozide. Patients were also excluded if they were unable to cooperate or judged by an investigator to be unfit for participation in the study.
Chemotherapy
The patients received the following regimens: FEC (5FU 500–600 mg/m2, epirubicin 100 mg/m2, and cyclophosphamide 500–600 mg/m2), EC (epirubicin 75 mg/m2 and cyclophosphamide 600 mg/m2), or AC (doxorubicin 60 mg/m2 and cyclophosphamide 600 mg/m2).
Study design and treatment schedule
This was a phase II, single-center, single-blind, placebo-controlled, parallel, randomized trial. Patients were randomized in a 1:1 ratio using a minimization method, with stratification into either arm A or arm B at the first cycle of chemotherapy. The patients in arm A received palonosetron (0.75 mg intravenously) plus dexamethasone (12 mg intravenously) and aprepitant (125 mg orally) on day 1, followed by dexamethasone (8 mg intravenously) and aprepitant (80 mg orally) on days 2 and 3. The patients in arm B received saline (as placebo, intravenously) instead of dexamethasone on days 2 and 3. Palonosetron, dexamethasone, and placebo were each dissolved in 50 mL of saline solution that was administered intravenously. The stratification factors included age (<50 years or ≥50 years) and type of HEC (FEC or AC/EC). To evaluate the efficacy endpoints of this study, every patient stayed for a minimum of 5 days in our hospital.
Assessments
The primary endpoint of this study was the proportion of patients with a complete response (CR), which was defined as no emetic episodes and no rescue medication during the overall phase (days 1–5). Secondary endpoints included the proportion of patients with a complete response during the delayed phase (days 2–5), the proportion of patients with complete control (CC: no emetic episodes, no rescue medication, and no more than mild nausea) during the overall phase, and the safety of these antiemetic therapies. The severity of nausea was categorized as none, mild, moderate, or severe, based on the subjective assessment of each patient. Any episode of nausea and vomiting was recorded in a diary contained in each patient self report. Investigators also assessed the number of emetic episodes and use of rescue medication by examining each patient’s nursing records. Adverse events and concomitant medication were recorded during the 5 days. Drug-related adverse events were classified according to NCI CTCAE, version 4.0. The full analysis set included all registered patients except those who were deemed ineligible after registration and those who withdrew their agreement. The endpoints were analyzed using the full analysis set. This study was performed according to the guidelines of the Declaration of Helsinki, as amended in Edinburgh, Scotland in October 2000. Institutional review board approval and written informed consents from the patients were obtained before any specific study procedures were begun.
Statistical analysis
A previous phase 3 clinical trial (PROTECT) found that the CR rate for palonosetron and dexamethasone 3 days treatment during the overall phase was 51.5 % [11]. Grote et al. has reported that the CR rate for palonosetron and dexamethasone and aprepitant treatment was 78 % [12]. Herrington et al. has reported that the CR rate was increased from 31.2 to 51.9 % when aprepitant was added to palonosetron and dexamethasone treatment [13]. Thus, the additional effect contributed by aprepitant was approximately 20 % [12–15]. Assuming a threshold CR rate of 50 % based on the previous study, an expected CR rate of 70 %, and with a one-sided α = 0.05 and β = 0.20, we calculated that each arm required 36 patients. Predicting that approximately 10 % of all patients would be excluded or withdrawn from the study, we determined that at least 40 patients were needed per arm.
A 90 % confidence interval (CI) was determined for the CR and CC rates. Comparisons were performed using a two-sided chi-square test. In addition to determining the CR rates of each treatment arm, subgroup analysis was performed to determine stratified CR rates during the overall phase.
JMP software (SAS Institute Inc., Cary, NC, USA) was used for statistical analysis. Statistical significance was considered to be p < 0.05.
Results
Patient characteristics (Table 1)
From April 2011 to June 2013, a total of 82 breast cancer patients treated at our hospital were enrolled in this trial. Two patients were excluded from the full analysis set. One patient had received previous chemotherapy, and the other patient withdrew her agreement to participate. The overview of patient characteristics is shown in Table 1. Forty one patients were assigned to arm A, and 39 patients were assigned to arm B. The characteristics of the patients were balanced between the groups.
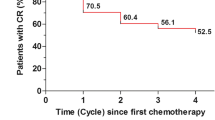
Complete response (Fig. 1a)
The overview of CR and CC is shown in Fig. 1. CRs for the overall phase were observed in 34/41 (82.9 %, 90 % CI 71.3–90.5 %) patients of arm A and 32/39 (82.1 %, 90 % CI 70.0–90.0 %; p = 1.00) patients of arm B. CRs for the delayed phase were 36/41 (87.8 %, 90 % CI 77.0–93.9 %) patients of arm A and 37/39 (94.9 %, 90 % CI 85.6–98.3 %; p = 0.43) patients of arm B.
Complete control (Fig. 1b)
CCs for the overall phase were observed in 20/41 (48.8 %, 90 % CI 36.4–61.3 %) patients of arm A and 24/39 (61.5 %, 90 % CI 48.4–73.2 %; p = 0.27) patients of arm B.
Complete responses in overall phase (subgroup analysis)
Among the younger patients (<50 years, n = 35), the CRs of arms A and B were 13/17 (76.5 %) and 14/18 (77.8 %), respectively (p = 1.00) (Fig. 2a). The CRs of the older patients (≥50 years, n = 45) of arms A and B were 21/24 (87.5 %) and 18/21 (85.7 %), respectively (p = 1.00) (Fig. 2a). The CRs of patients undergoing the AC/EC regimen (n = 32) of arms A and B were 16/17 (94.1 %) and 12/15 (80.0 %), respectively (p = 0.32) (Fig. 2b). The CRs of patients undergoing the FEC regimen (n = 48) of arms A and B were 18/24 (75.0 %) and 20/24 (83.3 %), respectively (p = 0.72) (Fig. 2b).
The relationship between the complete response rates of patients receiving dexamethasone days 1–3 (arm A) and patients receiving dexamethasone day 1 only (arm B), subgroup analyses. Two-sided chi-square test. Patients were stratified by (a) age, and (b) type of chemotherapy. AC anthracycline and cyclophosphamide, EC epirubicin and cyclophosphamide, FEC 5FU, epirubicin, and cyclophosphamide
Complete responses according to patient characteristics
The CRs for the overall phase of the younger and older patients were 27/35 (77.1 %) and 39/45 (86.7 %), respectively (p = 0.38) (Fig. 3a). The CRs for the overall phase of the patients undergoing the AC/EC and FEC regimens were 28/32 (87.5 %) and 38/48 (79.2 %), respectively (p = 0.92) (Fig. 3b).
The relationship between the complete response rates of patients receiving dexamethasone days 1–3 (arm A) and patients receiving dexamethasone day 1 only (arm B), patient’s characteristics analyses. Two-sided chi-square test. Patients were stratified by (a) age, and (b) type of chemotherapy. AC anthracycline and cyclophosphamide, EC epirubicin and cyclophosphamide, FEC 5FU, epirubicin, and cyclophosphamide
Safety
There were very few adverse events associated with either antiemetic regimen. Grade1 erythema was observed on the face of one patient in arm A after dexamethasone was infused. One patient in arm A had grade 1 generalized fatigue that might have been associated with chemotherapy. One patient in arm B had grade 1 headache, and 1 patient in arm B had grade 1 constipation. No severe adverse events attributed to antiemetic therapy were seen. Clinically abnormal laboratory values (white blood cell counts, neutrophil counts, platelet counts, hemoglobin, AST, ALT) that were attributed to chemotherapy developed in 73 patients.
Discussion
This study was the first phase II trial of breast cancer patients who received an HEC regimen and aprepitant and palonosetron. The trial evaluated the differences in the antiemetic effects of steroids administered for the standard duration and for a shorter duration of time. If no differences were seen in the antiemetic effects, the results would indicate that steroids could be administered for a shorter time, thereby reducing the side effects associated with steroids. The results show that the primary endpoints, CR for the overall phase, were equivalent (arm A: 82.9 %, 90 % CI 71.3–90.5 % vs arm B: 82.1 %, 90 % CI 70.0–90.0 %, p = 1.00). On the day of chemotherapy (day 1), conditions for both groups were the same, and a difference in the delayed phase was expected. However, the CR rates for the delayed phase were also equivalent (arm A; 87.8 %, 90 % CI 77.0–93.9 % vs arm B; 94.9 %, 90 % CI 85.6–98.3 %, p = 0.43).
Aapro et al. verified that 1 day of dexamethasone administration for breast cancer patients receiving chemotherapy was adequate [16]. They carried out a double-blind, randomized controlled study of 300 patients who received cyclophosphamide and/or anthracycline together with palonosetron (0.25 mg), with one arm receiving dexamethasone on day 1 and the other arm receiving dexamethasone on days 1–3. The results showed that the antiemetic effects were equivalent. They concluded that a 3-day regimen of steroids was not necessary when the second-generation 5-HT3 receptor antagonist palonosetron was administered. The overall CR rate was 53.6 % for the arm receiving dexamethasone on day 1 and 53.7 % for the arm receiving dexamethasone on days 1–3. The overall CR rates were higher in our study than in the Aapro study. Moreover, the CR rates of the acute and delayed phase were also higher in our study than the rates in the Aapro study. We think that the differences in CR rates might be attributed to the aprepitant therapy that was administered to our study patients. Another possible reason for the differences might be the differences in insurance-approved doses of palonosetron (0.75 mg in Japan vs 0.25 mg in other countries).
Regarding antiemetic treatments for the MEC regimens, Damien et al. carried out a single-arm phase II trial of 79 breast cancer patients who received AT (anthracycline, paclitaxel), palonosetron (0.25 mg), and steroids on day 1 only [17]. They found equivalent CC rates for the acute and delayed phases (77.6 and 73.7 %, respectively). Celio et al. carried out a phase III trial of 332 patients that included patients with breast cancer who received AC and palonosetron (0.25 mg) plus dexamethasone for 1 day or for 3 days [18]. The difference in the overall CR rates of those receiving dexamethasone for 1 or 3 days was not significant. The results of these trials suggest that with the administration of palonosetron during an MEC regimen, CINV can be controlled by 1 day of steroid administration. Moreover, Celio et al. performed a subgroup analysis [19]. Multivariate analysis determined that age younger than 50 years was a risk factor for CINV. The NCCN guidelines reported that the occurrence of acute emesis is affected by age and gender (female and younger patients [age < 50 years] are more prone to emesis). Our study found that there was no significant difference in the CRs of the younger and older patients (Fig. 3a).
In our study, the CC rates for the overall phase of arms A and B were 48.8 and 61.5 %, respectively. The CC rates were secondary endpoints, and the difference between arms A and B was not significant. However, the CC rate of arm B tended to be higher. The insignificant difference might be associated with the small sample and the fact that this was a subjective patient assessment.
The guidelines of the European Society of Medical Oncology, MASCC, ASCO, NCCN, and Japan Society of Clinical Oncology recommend that steroids be administered over several days to control CINV associated with HEC (www.jsco.or.jp) [20]. Although there were no severe adverse events due to steroid administration in our study, we think that for patients where CINV control is possible with aprepitant and palonosetron, decreased steroid use may be beneficial. Steroids should only be administered after considering their efficacy and side effects.
The results suggest that the antiemetic effect provided by dexamethasone administered for 3 days can be obtained by dexamethasone administered for 1 day for breast cancer patients who receive an HEC regimen. The small sample size was a major limitation of this study. However, we believe that a phase III study examining the utility of the 1 day dexamethasone treatment is warranted.
References
Feyer P, Jordan K (2011) Update and new trends in antiemetic therapy: the continuing need for novel therapies. Ann Oncol 22:30–38
Hesketh PJ, Kris MG, Grunberg SM, Beck T, Hainsworth JD, Harker G, Aapro MS, Gandara D, Lindley CM (1997) Proposal for classifying the acute emetogenicity of cancer chemotherapy. J Clin Oncol 15:103–109
Grunberg SM, Warr D, Gralla RJ, Rapoport BL, Hesketh PJ, Jordan K, Espersen BT (2011) Evaluation of new antiemetic agents and definition of antineoplastic agent emetogenicity—state of the art. Support Care Cancer 19(Suppl 1):S43–S47
American Society of Clinical O, Kris MG, Hesketh PJ, Somerfield MR, Feyer P, Clark-Snow R, Koeller JM, Morrow GR, Chinnery LW, Chesney MJ, Gralla RJ, Grunberg SM (2006) American Society of Clinical Oncology guideline for antiemetics in oncology: update 2006. J Clin Oncol 24:2932–2947
Tonini G, Vincenzi B, Santini D (2005) New drugs for chemotherapy-induced nausea and vomiting: focus on palonosetron. Expert Opin Drug Metab Toxicol 1:143–149
Gralla R, Lichinitser M, Van Der Vegt S, Sleeboom H, Mezger J, Peschel C, Tonini G, Labianca R, Macciocchi A, Aapro M (2003) Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron. Ann Oncol 14:1570–1577
Aapro MS, Grunberg SM, Manikhas GM, Olivares G, Suarez T, Tjulandin SA, Bertoli LF, Yunus F, Morrica B, Lordick F, Macciocchi A (2006) A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Ann Oncol 17:1441–1449
Vardy J, Chiew KS, Galica J, Pond GR, Tannock IF (2006) Side effects associated with the use of dexamethasone for prophylaxis of delayed emesis after moderately emetogenic chemotherapy. Br J Cancer 94:1011–1015
Yeo W, Chan PK, Zhong S, Ho WM, Steinberg JL, Tam JS, Hui P, Leung NW, Zee B, Johnson PJ (2000) Frequency of hepatitis B virus reactivation in cancer patients undergoing cytotoxic chemotherapy: a prospective study of 626 patients with identification of risk factors. J Med Virol 62:299–307
Yeo W, Zee B, Zhong S, Chan PK, Wong WL, Ho WM, Lam KC, Johnson PJ (2004) Comprehensive analysis of risk factors associating with Hepatitis B virus (HBV) reactivation in cancer patients undergoing cytotoxic chemotherapy. Br J Cancer 90:1306–1311
Saito M, Aogi K, Sekine I, Yoshizawa H, Yanagita Y, Sakai H, Inoue K, Kitagawa C, Ogura T, Mitsuhashi S (2009) Palonosetron plus dexamethasone versus granisetron plus dexamethasone for prevention of nausea and vomiting during chemotherapy: a double-blind, double-dummy, randomised, comparative phase III trial. Lancet Oncol 10:115–124
Grote T, Hajdenberg J, Cartmell A, Ferguson S, Ginkel A, Charu V (2006) Combination therapy for chemotherapy-induced nausea and vomiting in patients receiving moderately emetogenic chemotherapy: palonosetron, dexamethasone, and aprepitant. J Support Oncol 4:403–408
Herrington JD, Jaskiewicz AD, Song J (2008) Randomized, placebo-controlled, pilot study evaluating aprepitant single dose plus palonosetron and dexamethasone for the prevention of acute and delayed chemotherapy-induced nausea and vomiting. Cancer 112:2080–2087
Warr DG, Hesketh PJ, Gralla RJ, Muss HB, Herrstedt J, Eisenberg PD, Raftopoulos H, Grunberg SM, Gabriel M, Rodgers A, Bohidar N, Klinger G, Hustad CM, Horgan KJ, Skobieranda F (2005) Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol 23:2822–2830
Longo F, Mansueto G, Lapadula V, De Sanctis R, Quadrini S, Grande R, Gori B, Altavilla A, D’Antoni I, Del Signore E, Stumbo L, De Luca C, Cimadon B, Cortesi E, Gamucci T, Di Seri M Palonosetron plus 3-day aprepitant and dexamethasone to prevent nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer 19: 1159–1164
Aapro M, Fabi A, Nole F, Medici M, Steger G, Bachmann C, Roncoroni S, Roila F (2010) Double-blind, randomised, controlled study of the efficacy and tolerability of palonosetron plus dexamethasone for 1 day with or without dexamethasone on days 2 and 3 in the prevention of nausea and vomiting induced by moderately emetogenic chemotherapy. Ann Oncol 21:1083–1088
Damian S, Celio L, De Benedictis E, Mariani P, Agustoni F, Ricchini F, De Braud F (2013) Is a dexamethasone-sparing strategy capable of preventing acute and delayed emesis caused by combined doxorubicin and paclitaxel for breast cancer? analysis of a phase II trial. Oncology 84:371–377
Celio L, Frustaci S, Denaro A, Buonadonna A, Ardizzoia A, Piazza E, Fabi A, Capobianco AM, Isa L, Cavanna L, Bertolini A, Bichisao E, Bajetta E, Italian Trials in Medical Oncology G (2011) Palonosetron in combination with 1-day versus 3-day dexamethasone for prevention of nausea and vomiting following moderately emetogenic chemotherapy: a randomized, multicenter, phase III trial. Support Care Cancer 19:1217–1225
Celio L, Denaro A, Agustoni F, Bajetta E (2012) Palonosetron plus 1-day dexamethasone for the prevention of nausea and vomiting due to moderately emetogenic chemotherapy: effect of established risk factors on treatment outcome in a phase III trial. J Support Oncol 10:65–71
Jordan K, Gralla R, Jahn F, Molassiotis A (2014) International antiemetic guidelines on chemotherapy induced nausea and vomiting (CINV): content and implementation in daily routine practice. Eur J Pharmacol 722:197–202
Acknowledgments
We would like to thank all of the patients who participated in this study and their families, as well as the investigators and research nurses.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kosaka, Y., Tanino, H., Sengoku, N. et al. Phase II randomized, controlled trial of 1 day versus 3 days of dexamethasone combined with palonosetron and aprepitant to prevent nausea and vomiting in Japanese breast cancer patients receiving anthracycline-based chemotherapy. Support Care Cancer 24, 1405–1411 (2016). https://doi.org/10.1007/s00520-015-2905-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-015-2905-4