Abstract
Purpose
The purpose of this study was to report the opinions and self-reported practices of clinicians, as well as the availability of decision support tools, regarding appropriate thromboprophylaxis for patients with lung cancer to identify variation in practice and/or divergence from evidence-based clinical practice guidelines (CPG).
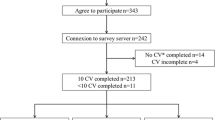
Methods
A computer-generated survey (SurveyMonkey software) was distributed to surgical, radiation and medical oncologists with lung cancer specialisation, via membership of the Australian Lung Cancer Trials Group (ALTG) from May to September 2013.
Results
Seventy-two clinicians, from public, private, specialist and general hospitals, completed the survey (46 % response rate). Hospital-endorsed CPG were widely available (91 %); however, these routinely lacked robust recommendations for the ambulatory care setting (98 %) and risk stratification tools (65 %). Clinicians consistently identified ambulatory care treatment modalities (chemotherapy, alone or in combination with radiotherapy) as having similar (high) thrombotic risk as surgery. Timing and duration of pharmacological thromboprophylaxis prescribing among surgical oncologists varied and were divergent from guideline recommendations. Fifty-eight percent of surveyed clinicians cited a lack of high-quality data to guide preventative strategies in lung cancer patients.
Conclusion
Clinicians consistently identified patients with lung cancer as having a high thromboembolic risk in both ambulatory and surgical settings, but with differences in recommendations and variation in practice. CPG lacked robust recommendations for the ambulatory care setting, the main arena for the multimodality lung cancer treatment paradigm.



Similar content being viewed by others
Reference List
GLOBOCAN 2008. Lung cancer incidence and mortality worldwide in 2008. International Agency for Research on Cancer. World Health Organisation. Accessed 10/10/13. Available: http://globocan.iarc.fr/factsheets/cancers/lung.asp
Rickles FR, Edwards RL (1983) Activation of blood coagulation in cancer: Trousseau’s syndrome revisited. Blood 62(1):14–31
Corrales-Rodriguez L, Blais N (2012) Lung cancer associated venous thromboembolic disease: a comprehensive review. Lung cancer (Amsterdam, Netherlands) 75(1):1–8
Connolly GC, Dalal M, Lin J, Khorana AA (2012) Incidence and predictors of venous thromboembolism (VTE) among ambulatory patients with lung cancer. Lung cancer 78(3):253–258
Huang H, Korn JR, Mallick R, Friedman M, Nichols C, Menzin J (2012) Incidence of venous thromboembolism among chemotherapy-treated patients with lung cancer and its association with mortality: a retrospective database study. J Thromb Thrombolysis 34(4):446–456
Lamy A, Wang X, Kent R, Smith KM, Gafni A (2002) Economic evaluation of the MEDENOX trial: a Canadian perspective. Medical patients with enoxaparin. Can Respir J 9(3):169–177
Bergqvist D (2002) Enoxaparin: a pharmacoeconomic review of its use in the prevention and treatment of venous thromboembolism and in acute coronary syndromes. Pharmacoeconomics 20(4):225–243
Khorana AA, Streiff MB, Farge D, Mandala M, Debourdeau P, Cajfinger F, Marty M, Falanga A, Lyman GH (2009) Venous thromboembolism prophylaxis and treatment in cancer: a consensus statement of major guidelines panels and call to action. J Clin Oncol 27(29):4919–4926
Leavitt MO (2008) The surgeon general's call to action to prevent deep vein thrombosis and pulmonary embolism. U.S. Department of Health and Human Services (HHS) under the direction of the Office of the Surgeon General and the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health. Accessed 10/10/13. Available: http://www.surgeongeneral.gov/library/calls/deepvein/call-to-action-on-dvt-2008.pdf
Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B, Huang W, Zayaruzny M, Emery L, Anderson FA Jr (2008) Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 371(9610):387–394
Chew HK, Davies AM, Wun T, Harvey D, Zhou H, White RH (2008) The incidence of venous thromboembolism among patients with primary lung cancer. J Thromb Haemost 6(4):601–608. doi:10.1111/j.1538-7836.2008.02908.x
Horsted F, West J, Grainge MJ (2012) Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLoS Med 9(7):e1001275. doi:10.1371/journal.pmed.1001275
Hicks LK, Cheung MC, Ding K, Hasan B, Seymour L, Le Maitre A, Leighl NB, Shepherd FA (2009) Venous thromboembolism and nonsmall cell lung cancer: a pooled analysis of National Cancer Institute of Canada Clinical Trials Group trials. Cancer 115(23):5516–5525
Agnelli G, Gussoni G, Bianchini C, Verso M, Mandala M, Cavanna L, Barni S, Labianca R, Buzzi F, Scambia G, Passalacqua R, Ricci S, Gasparini G, Lorusso V, Bonizzoni E, Tonato M (2009) Nadroparin for the prevention of thromboembolic events in ambulatory patients with metastatic or locally advanced solid cancer receiving chemotherapy: a randomised, placebo-controlled, double-blind study. Lancet Oncol 10(10):943–949
Haas SK, Freund M, Heigener D, Heilmann L, Kemkes-Matthes B, von Tempelhoff GF, Melzer N, Kakkar AK (2012) Low-molecular-weight heparin versus placebo for the prevention of venous thromboembolism in metastatic breast cancer or stage III/IV lung cancer. Clin Appl Thromb Hemost 18(2):159–165
Macbeth F, Noble S, Griffiths G, Chowdhury R, Rolfe C, Hood K, Linnane S, Moore B, Cohen D, Cowles R, Longo M, Knoyle D (2013) Preliminary results from the FRAGMATIC trial: a randomised phase III clinical trial investigating the effect of FRAGMin® added to standard therapy in patients with lung cancer [conference abstract MO27.02]. J Thorac Oncol 8, Supplement 2
Lyman GH, Khorana AA, Kuderer NM, Lee AY, Arcelus JI, Balaban EP, Clarke JM, Flowers CR, Francis CW, Gates LE, Kakkar AK, Key NS, Levine MN, Liebman HA, Tempero MA, Wong SL, Prestrud AA, Falanga A (2013) Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. doi:10.1200/jco.2013.49.1118
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, Colwell CW (2008) Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest 133(6 Suppl):381S–453S
Mandalà M, Falanga A, Roila F, Group ObotEGW (2011) Management of venous thromboembolism (VTE) in cancer patients: ESMO clinical practice guidelines. Ann Oncol 22(6):vi85–vi92. doi:10.1093/annonc/mdr392
National Institute for Health and Care Excellence (NICE) Clinical Guideline 92 (2010) Venous thromboembolism: reducing the risk. National Collaborating Centre for Acute and Chronic Conditions, London
National Health and Medical Research Council (NHMRC) (2009) Clinical practice guideline for the prevention of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to Australian hospitals. National Health and Medical Research Council, Melbourne
Australia and New Zealand Working Party on the Management and Prevention of Venous Thromboembolism (2007) Prevention of ve-nous thromboembolism: best practice guidelines for Australia and New Zealand, 4th edn. Health Education and Management Innovations, Sydney
Streiff MB (2010) The National Comprehensive Cancer Center Network (NCCN) guidelines on the management of venous thromboembolism in cancer patients. Thromb Res 125(2):S128–S133
Farge D, Debourdeau P, Beckers M, Baglin C, Bauersachs RM, Brenner B, Brilhante D, Falanga A, Gerotzafias GT, Haim N, Kakkar AK, Khorana AA, Lecumberri R, Mandala M, Marty M, Monreal M, Mousa SA, Noble S, Pabinger I, Prandoni P, Prins MH, Qari MH, Streiff MB, Syrigos K, Bounameaux H, Buller HR (2013) International clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. J Thromb Haemost 11(1):56–70. doi:10.1111/jth.12070
Siragusa S, Armani U, Carpenedo M, Falanga A, Fulfaro F, Imberti D, Laurora R, Molinari AC, Prisco D, Silingardi M, Verso M, Visona A (2012) Prevention of venous thromboembolism in patients with cancer: guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thromb Res 129(5):e171–e176
Scarci M, Pilling J, Harrison-Phipps K, Tennyson C, Routledge T (2010) Right upper video-assisted thoracoscopic lobectomy for early stage lung cancer. Multimed Man Cardiothorac Surg. doi:10.1510/mmcts.2009.004333
Gagarine A, Urschel JD, Miller JD, Bennett WF, Young JE (2003) Preoperative and intraoperative factors predictive of length of hospital stay after pulmonary lobectomy. Ann Thorac Cardiovasc Surg 9(4):222–225
Wright CD, Gaissert HA, Grab JD, O’Brien SM, Peterson ED, Allen MS (2008) Predictors of prolonged length of stay after lobectomy for lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database risk-adjustment model. Ann Thorac Surg 85(6):1857–1865. doi:10.1016/j.athoracsur.2008.03.024
Ay C, Dunkler D, Simanek R, Thaler J, Koder S, Marosi C, Zielinski C, Pabinger I (2011) Prediction of venous thromboembolism in patients with cancer by measuring thrombin generation: results from the Vienna Cancer and Thrombosis Study. J Clin Oncol 29(15):2099–2103. doi:10.1200/jco.2010.32.8294
Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111(10):4902–4907
Ay C, Dunkler D, Marosi C, Chiriac AL, Vormittag R, Simanek R, Quehenberger P, Zielinski C, Pabinger I (2010) Prediction of venous thromboembolism in cancer patients. Blood 116(24):5377–5382. doi:10.1182/blood-2010-02-270116
Alexander M, Teoh KC, Lingaratnam S, Kirsa S, Mellor JD (2013) Thromboprophylaxis prescribing and thrombotic event rates in multiple myeloma patients treated with lenalidomide or thalidomide at a specialist cancer hospital. Asia Pac J Clin Oncol 9(2):169–175. doi:10.1111/ajco.12013
Watts AC, Brenkel IJ (2005) A postal survey of current thromboprophylactic practices of consultant orthopaedic surgeons in the treatment of fracture of the hip. J Bone Joint Surg (Br) 87-B(3):296–300. doi:10.1302/0301-620x.87b3.15060
Filtenborg Tvedskov T, Rasmussen MS, Wille-Jorgensen P (2001) Survey of the use of thromboprophylaxis in laparoscopic surgery in Denmark. Br J Surg 88(10):1413–1416
Bryson DJ, Uzoigwe CE, Braybrooke J (2012) Thromboprophylaxis in spinal surgery: a survey. J Orthop Surg Res 7:14
Molnar RB, Jenkin DE, Millar MJ, Campbell D, Harris IA (2012) The Australian arthroplasty thromboprophylaxis survey. J Arthroplasty 27(2):173–179
Srinivasaiah N, Arsalani-Zadeh R, Monson JR (2012) Thrombo-prophylaxis in colorectal surgery: a National Questionnaire Survey of the members of the Association of Coloproctology of Great Britain and Ireland. Colorectal Dis 14(7):e390–e393. doi:10.1111/j.1463-1318.2012.02974.x
Smart P, Burbury K, Lingaratnam S, Lynch AC, Mackay J, Heriot A (2012) Thromboprophylaxis among Australasian colorectal surgeons. ANZ J Surg 83(9):646–650
Wolff RA (2003) Are patients with cancer receiving adequate thromboprophylaxis? Results from FRONTLINE. Cancer Treat Rev 2:7–9
Hopkins L, Carrier M, Plante M, Luna V, Gotlieb W, Rambout L (2012) Surgical venous thromboprophylaxis: a cross-sectional survey of Canadian gynaecologic oncologists. J Obstet Gynaecol Can 34(7):673–677
Cavaliere L (2013) Thromboprophylaxis in ambulatory lung cancer treatment. Clin J Oncol Nurs 17(1):74–79. doi:10.1188/13.cjon.74-79
Sousou T, Khorana AA (2010) Cancer patients and awareness of venous thromboembolism. Cancer Invest 28(1):44–45. doi:10.3109/07357900902744544
Rose AJ, Sharman JP, Ozonoff A, Henault LE, Hylek EM (2007) Effectiveness of warfarin among patients with cancer. J Gen Intern Med 22(7):997–1002. doi:10.1007/s11606-007-0228-y
Acknowledgments
The authors would like to acknowledge the support of the Australian Lung Cancer Trials Group in the distribution of the survey and to thank the clinicians who participated.
Conflict of interest
None
Funding
None declared
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alexander, M., Kirsa, S., MacManus, M. et al. Thromboprophylaxis for lung cancer patients—multimodality assessment of clinician practices, perceptions and decision support tools. Support Care Cancer 22, 1915–1922 (2014). https://doi.org/10.1007/s00520-014-2170-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2170-y