Abstract
Purpose
This project sought to help palliative and hospice care practices improve patient care quality and operational efficiency by improving patient symptom status reporting and symptom management, reducing associated provider documentation workload, and enhancing patient–provider and provider–provider communication. We developed a user-friendly, electronic medical record-compatible, software prototype that allows typical clinical data and patient-reported outcomes (PRO) to be entered and stored. This data is immediately available during the clinical encounter with graphically depicted summaries for patient history and PRO assessments, a trending feature that links symptom behavior to interventions and the Edmonton Labeled Visual Information System.
Methods
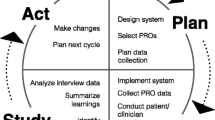
A user-centered design approach allowed for iterative cycles of needs/usability feedback from providers and patients/caregivers to be incorporated into the development of our prototype’s technical structure and features. To determine the needs and initial usability of the project’s prototype, we interviewed eight providers and 18 patients/caregivers. Another usability test, consisting of patient/caregiver (n = 18) and provider (n = 9) interviews, assessed the functioning prototype’s design, usability, and usefulness.
Results
Patients/caregivers (n = 18) reported that the prototype was usable (100%), it would facilitate patient–provider communication, shared decision making, and self-management (100%), and they would be willing to try the system and recommend it to their providers (100%). The providers (n = 9) felt that the prototype encouraged better use of patient assessments in decision making and patient care (100%) and improved identification of cause/temporal relationship between care events and outcomes (100%), monitoring of patient status (100%), communication in a multi-disciplinary team (100%), and operational efficiency and patient care quality (88.9%).
Conclusions
Quality of patient care and operational efficiency can be improved with an effective assessment, evaluation, and communication tool. This project developed an electronic version of such a tool. Future efforts will hone its usability and integration across multiple hospice/palliative care settings.



Similar content being viewed by others
References
Naccache N, Abou Zeid H, Nasser Ayoub E, Antakly MC (2008) Pain management and health care policy. J Méd Liban 56(2):105–111
Downing J (2008) The conception of the Nankya model of palliative care development in Africa. Int J Palliat Nurs 14(9):459–464
Lim R (2008) Improving cancer pain management in Malaysia. Oncology 74(Suppl 1):24–34
Tueni E (2008) Perspectives in palliative care? J Méd Liban 56(2):129–131
SUPPORT Principal Investigators, Connors AF Jr, Dawson NV et al (1995) A controlled trial to improve care for seriously III hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT). JAMA 274(20):1591–1598
Pritchard RS, Fisher ES, Teno JM et al (1998) Influence of patient preferences and local health system characteristics on the place of death. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Risks and Outcomes of Treatment. J Am Geriatr Soc 46(10):1242–1250
Covinsky KE, Fuller JD, Yaffe K et al (2000) Communication and decision-making in seriously ill patients: findings of the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc 48(5 Suppl):S187–S193
Cherlin E, Fried T, Prigerson HG, Schulman-Green D, Johnson-Hurzeler R, Bradley EH (2005) Communication between physicians and family caregivers about care at the end of life: when do discussions occur and what is said? J Pall Med 8(6):1176–1185
Middlewood S, Gardner G, Gardner A (2001) Dying in hospital: medical failure or natural outcome? J Pain Symptom Manage 22(6):1035–1041
Field MJ, Cassel CK (2001) Institute of Medicine. Committee on Care at the End of L, NetLibrary I. Approaching death improving care at the end of life. Washington, DC: National Academy Press
Breitbart W, Rosenfeld B, Roth A, Smith MJ, Cohen K, Passik S (1997) The memorial delirium assessment scale. J Pain Symptom Manage 13(3):128–137
Lawlor PG, Nekolaichuk C, Gagnon B, Mancini IL, Pereira JL, Bruera ED (2000) Clinical utility, factor analysis, and further validation of the memorial delirium assessment scale in patients with advanced cancer: assessing delirium in advanced cancer. Cancer 88(12):2859–2867
Fainsinger RL, Nekolaichuk CL (2008) A “TNM” classification system for cancer pain: the Edmonton Classification System for Cancer Pain (ECS-CP). Support Care Cancer 16(6):547–555
Nekolaichuk CL, Fainsinger RL, Lawlor PG (2005) A validation study of a pain classification system for advanced cancer patients using content experts: the edmonton classification system for cancer pain. Palliat Med 19(6):466–476
Ewing JA (1984) Detecting alcoholism. The CAGE questionnaire. Jama 252(14):1905–1907
Mayfield D, McLeod G, Hall P (1974) The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry 131(10):1121–1123
Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K (1991) The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 7(2):6–9
Chang VT, Hwang SS, Feuerman M (2000) Validation Edmonton Symptom Assess Scale Cancer 88(9):2164–2171
Walker P, Nordell C, Cace S, Neumann CM, Bruera E (2001) Impact of the Edmonton Labeled Visual Information System on physician recall of metastatic cancer patient histories. a randomized controlled trial. J Pain Symptom Manage 21(1):4–11
Schensul SL, Schensul JJ, LeCompte MD (1999) Essential ethnographic methods: observations, interviews, and questionnaires. AltaMira, Walnut Creek
LeCompte MD, Schensul JJ (1999) Analyzing and interpreting ethnographic data. AltaMira, Walnut Creek
LeCompte MD, Schensul JJ (1999) Designing and conducting ethnographic research. AltaMira Press, Walnut Creek
Brooke J (2009) The system usability scale: a quick and dirty usability scale; http://www.usabilitynet.org/trump/documents/Suschapt.doc. Accessed June 15, 2010.
Bangor A (2009) Determining what individual SUS scores mean: adding an adjective rating scale. Journal of Usability Studies 4(3):114–123
Acknowledgment
This project has been funded in whole with Federal funds from the National Cancer Institute, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN261200800050C and NCI Control No. N43CO-2008-00050.
Conflict of interest
Authors Yang and Haas are the developers of this product and work for BrightOutcome.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kallen, M.A., Yang, D. & Haas, N. A technical solution to improving palliative and hospice care. Support Care Cancer 20, 167–174 (2012). https://doi.org/10.1007/s00520-011-1086-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-011-1086-z