Abstract
Goal
The goal of this study was to characterize the sleep problems of children with cancer who were referred for a comprehensive sleep evaluation.
Materials and methods
A retrospective case series review was conducted of all children with cancer referred to the pediatric sleep clinic from 1994 to 2009 for evaluation of a sleep problem. Seventy children were seen and evaluated during this interval; all had a complete sleep history taken, and further objective sleep evaluations were performed as part of their evaluation only when clinically indicated. An overnight polysomnogram was performed in 53 children. In 36 children with a history of excessive daytime sleepiness (EDS), a multiple sleep latency study was performed the following day. Seven children had a 3–4-week actigraphic study.
Results
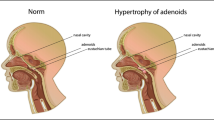
Children with neoplasms of central nervous system (CNS) involving the hypothalamus, thalamus, and brainstem were the most commonly referred children and had the most frequent and severe sleep problems. Excessive daytime sleepiness was the most common sleep problem, seen in 60% of children with cancer and in 80% of children with CNS neoplasms involving the hypothalamus, thalamus, and brainstem. Sleep disordered breathing (SDB) was present in 40% of the entire group of children with cancer and 46% of children with neoplasms involving the hypothalamus, thalamus, and brainstem. Children with CNS neoplasms often had more than one sleep problem, most commonly EDS and SDB. In these children, correction of the SDB often did not eliminate the EDS. In children with leukemia, insomnia was the most common sleep problem identified, present in 39%. The causes of the sleep problems were varied and included neurologic injury caused by the neoplasm and/or the CNS-directed treatments; seizures, adenotonsillar hypertrophy, medication side effects, obesity, pain, anxiety, and drug abuse. Some of the sleep problems were present before the diagnosis of cancer, though most developed after treatment was begun. A wide range of intervention strategies were utilized to address the sleep problems and included sleep hygiene/sleep restriction, behavioral counseling, continuous positive airway pressure, bilevel positive airway pressure, tracheotomy with and without a ventilator, diaphragmatic pacers, sedative hypnotics, stimulants, anticonvulsants, and antidepressants. When the sleep problems and their causes were correctly identified and treatments were directed to the specific cause of the problem, the treatments were generally successful.
Conclusions
The sleep problems of children with cancer span the full spectrum of clinical sleep disorders (hypersomnia, sleep disordered breathing, insomnia, parasomnias, and circadian rhythm disorders) and are often present in combinations. Children with neoplasms involving the brainstem, thalamus, and hypothalamus were the most frequently referred for a sleep evaluation, and their sleep problems were most commonly EDS or SDB. Expertise in pediatric sleep disorders can be a valuable resource in the ongoing care of children with cancer.

Similar content being viewed by others
References
Saper C, Scammell T, Lu J (2005) Hypothalamic regulation of sleep and circadian rhythms. Nature 437:1257–1263
Muller H, Handwerker G, Gebhardt U et al (2007) Melatonin treatment in obese patients with craniopharyngioma and increased sleepiness. Cancer Causes Control 17:583–589
Puget S, Garnett M, Wray A et al (2007) Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg Pediatr 106:3–12
Benesch M, Lackner H, Sovinz P et al (2006) Late sequela after treatment of childhood low-grade gliomas: a retrospective analysis of 69 long term survivors treated between 1983 and 2003. J Neuro-oncol 78:199–205
Wilne S, Collier J, Kennedy C et al (2007) Presentation of childhood CNS tumors: a systematic review and meta-analysis. Lancet Oncol 8:685–695
Rosen GM, Bendel AE, Neglia JP, Moertel CL, Mahowald M (2003) Sleep in children with neoplasms of the central nervous system: case review of 14 children. Pediatrics 112(1):e46–e54
Nishino S, Kanbayashi T (2005) Symptomatic narcolepsy, cataplexy and hypersomnia, and their implications in the hypothalamic hypocretin/orexin system. Sleep Med Rev 9:269–310
Palm L, Nordin V, Elmquist D et al (1992) Sleep and wakefulness after treatment for craniopharyngioma in childhood; influence on the quality and maturation of sleep. Neuropediatrics 23:39–45
Someren E, Swart-Heikens J, Endert E et al (2004) Long term effect of cranial irradiation for childhood malignancy on sleep in adulthood. European J Endo 150:503–510
Ryan J (2000) Radiation somnolence syndrome. J Pediatr Oncol Nurs 17:50–53
Faithful S, Brada M (1998) Somnolence syndrome in adults following cranial irradiation for primary brain tumors. Clin Oncol 10:250–254
Mindell J, Owens J (2003) A clinical guide to pediatric sleep, diagnosis and management of sleep problems. Lippincott, Philadelphia
Jenni OG, Carscadon MA (2007) Sleep behavior and sleep regulation from infancy through adolescence: normative aspects. Sleep Med Clin 2:321–329
Carscadon MA, Acebo A (2002) Regulation of sleepiness in adolescents: updates, insights, and speculation. Sleep 25(6):606–614
Iglowstein I, Jenni O, Molinari L et al (2003) Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 111:302–307
Mindell J, Kuhn B, Lewin D et al (2006) Behavioral treatments of bedtime problems and night wakings in infants and young children. Sleep 29(10):1263–1276
Owens J (2005) In: Sheldon S, Ferber R, Kryger M (eds) Principles and practice of pediatric sleep medicine. Elsevier, Philadelphia, pp 27–34
Brooks L (2005) Obstructive sleep apnea syndrome in infants and children: clinical features and pathophysiology. In: Sheldon S, Ferber R, Kryger M (eds) Principles and practice of pediatric sleep medicine. Elsevier, Philadelphia, pp 223–231
Rosen G (2005) Evaluation of the patient who has sleep complaints: a case based method using the sleep process matrix. Prim Care Clin Office Pract 32:319–328
American Cancer Society (2007) Cancer facts and figures 2007. http://www.cancer.org/downloads/STT/CAFF2007PWSecured.pdf
CBTRUS Central (2005) Statistical report: primary brain tumors in the United States, 1998–2002. Central Brain Tumor Registry of the United States, Hinsdale
Oeffinger K, Mertens A, Sklar C et al (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355(15):1572–1582
Gurney JG, Kadan-Lottick NS, Packer RJ et al (2003) Endocrine and cardiovascular late effects among adult survivors of childhood brain tumors. Childhood Cancer Survivor Study. Cancer 97(3):663–673
Mulhern RK, Merchant TE, Wallace D, Kocak M, Brouwers P, Krull K, Chintagumpala M, Stargatt R, Ashley DM, Tyc VL, Kun L, Boyett J, Gajjar A (2005) Neurocognitive consequences of risk adapted therapy for childhood medulloblastoma. J Clin Oncol 23(24):5511–5519
Ancoli-Israel A, Moore P, Jones V (2001) The relationship between fatigue and sleep in cancer patients: a review. Eur J Cancer Care 10:245–255
Iber C, Ancoli-Israel S, Chesson A, Quan S (2007) The AASM manual for the scoring of sleep and associated disorders. AASM, Westchester
Hauri P, Sateia M (2005) The international classification of sleep disorders diagnostic and coding manual, 2nd edn. AASM, Westchester
Littner M, Kushida C, Anderson W et al (2003) Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep 26:337–341
Littner M, Kushida C, Wise M et al (2005) Practice parameters in the clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 28:113–121
Hinds P, Hockenberry M, Gattuso J et al (2007) Dexamethasone alters sleep and fatigue in pediatric patients with acute lymphoblastic leukemia. Cancer 110:2321–2330
Savard J, Liu L, Natarajan L, Rissling MB, Neikrug AB, He F, Dimsdale JE, Mills PJ, Parker BA, Sadler GR, Ancoli-Israel S (2009) Breast cancer patients have progressively impaired sleep–wake activity rhythms during chemotherapy. Sleep 32:1155–1160
Dupuis L, Milne-Wren C, Cassidy M et al (2010) Symptom assessment in children receiving cancer therapy: the parents perspective. Support Care Cancer 18:281–299
Meeske K, Katz E, Palmer S et al (2004) Parent proxy-reported health related quality of life and fatigue in pediatric patients diagnosed with brain tumors and acute lymphoblastic leukemia. Cancer 101:2116–2125
Acknowledgement
This work could not have been completed without the advice and support of Dr. Mark Mahowald.
Conflicts of interest
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosen, G., Brand, S.R. Sleep in children with cancer: case review of 70 children evaluated in a comprehensive pediatric sleep center. Support Care Cancer 19, 985–994 (2011). https://doi.org/10.1007/s00520-010-0921-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0921-y