Abstract
Goals of work
The objective of the study is to assess the Palliative Care Outcome Scale (POS) as a potential audit tool within a specialist cancer centre. It also aims to answer the following questions: does the tool identify problem areas and demonstrate changes in quality of life over time? How well do staff and patient ratings correlate?
Patients and methods
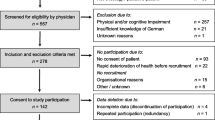
The POS questionnaire was piloted at a specialist cancer centre. Thirty consecutive patients admitted to the palliative care wards and ward staff completed questionnaires on admission and twice weekly until discharge or death. A further questionnaire assessed staff attitudes.
Results
There was a significant improvement in overall patient POS score at 1 week (days 5–9). Four “symptoms” or issues were scored as being important for our patients: pain, other symptoms, anxiety and patient’s perception of family anxiety. These all significantly improved within the first week. At the initial assessment, staff underestimated patients’ pain and overestimated problems relating to information giving and patients’ ability to share their feelings. There was no significant difference between staff and patient scores after 1 week. The other six areas covered by the tool were less important; this may reflect the patient population seen at our centre. Use of the tool identified areas for staff training and effectively demonstrated improvement in patient care.
Conclusion
The POS is an outcome measure tool designed to assess physical, psychological, practical and existential aspects of quality of life. It may be useful in identifying problems in individual patients and directing care to address these needs.

Similar content being viewed by others
References
Hearn J, Higginson IJ (1997) Outcome measures in palliative care for advanced cancer patients: a review. J Public Health Med 19(2):193–199
Hearn J, Higginson IJ (1999) Development and validation of a core outcome measure for palliative care: the palliative care outcome scale. Qual Health Care 8:219–227
Rees E, Hardy J, Ling J, Broadley K, A’Hern R (1998) The use of the Edmonton Symptom Assessment Scale (ESAS) within a palliative care unit in the UK. Palliat Med 12:75–82
Hardy J, Edmonds P, Turner R, Rees E, A’Hern R (1999) The use of the Rotterdam Symptom Checklist in Palliative Care. J Pain Symp Manag 18 (2):79–84
Slevin ML, Plant H, Lynch D, Drinkwater J, Gregory WM (1988) Who should measure quality of life, the doctor or the patient? Br J Cancer 57:109–112
Higginson IJ, McCarthy M (1993) Validity of the support team assessment schedule: do staff’s rating reflect those made by patients or their families? Palliat Med 7:219–228
Field D, Douglas C, Jagger C et al (1995) Terminal illness: views of patients and their lay carers. Palliat Med 9:45–54
Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M (2002) Dignity in the terminally ill: a cross-sectional, cohort study. Lancet 360:2026–2030
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stevens, AM., Gwilliam, B., A’Hern, R. et al. Experience in the use of the palliative care outcome scale. Support Care Cancer 13, 1027–1034 (2005). https://doi.org/10.1007/s00520-005-0815-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0815-6