Abstract
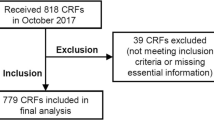
Consecutive cancer referrals to a palliative medicine program were evaluated to assess nutritional status using a standard protocol. The study included 352 patients (180 men, 172 women; median age 61 years, range 22–94 years). The most common diagnosis was lung cancer. All had metastatic disease, 139 with gastrointestinal involvement. The most common gastrointestinal symptoms were weight loss (n=307), anorexia (n=285), and early satiety (n=243). Of those with any weight loss, 71% had lost ≥10% of their pre-illness weight. The most common factor identified which might have contributed to weight loss was hypophagia (n=275/307). Men had lost weight more often and to a greater extent than women. Triceps skinfold (TSF) was measured in 337: 51% had values that suggested severe fat deficiency. Upper mid-arm muscle area (AMA) was measured in 349: 30% had evidence of significant muscle mass reduction. The body mass index (BMI) was normal or increased in most patients. Calculated resting energy expenditure (REE) (n=324) was high in 41%. C-reactive protein was elevated in 74% of those measured (n=50). We conclude that: (1) most of this group of cancer patients referred to palliative medicine had severe weight loss; (2) there was a gender difference in the severity and type of weight loss; (3) males lost more weight overall and more muscle than females; (4) males with any degree of weight loss had a higher REE than females; (5) a significant correlation existed between the time from diagnosis to death and the severity of weight loss in the prior month; (6) BMI was normal in most patients, suggesting precancer diagnosis obesity; and (7) both TSF and AMA correlated well with body composition of both fat and protein as determined by bioelectrical impedance.


Similar content being viewed by others
References
Abraham S, Carroll MD, Najjar MF, Fulwood R (1983) Obese and overweight adults in the United States. Vital Health Stat 11:1–93
Alpers DH, Stenson WF, Bier DM (1995) Protein and calories requirements, intake and assessment. In: Apers DH, Stenson WF, Bier DM (eds) Manual of nutrition therapy. Little, Brown and Company, Boston, MA, pp 73–114
Baker JP, Detsky AS, Wesson DE, et al (1982) Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med 306:969–972
Baker JP, Detsky AS, Whitwell J, Langer B, Jeejeebhoy KN (1982) A comparison of the predictive value of nutritional assessment techniques. Hum Nutr Clin Nutr 36:233–241
Baumann H, Gauldie J (1994) The acute phase response [see comments]. Immunol Today 15:74–80
Berry JK, Braunschweig CA (1998) Nutritional assessment of the critically ill patient. Crit Care Nurs Q 21:33–46
Blackburn G (1998) Wasting away: cancer cachexia. Health News 4:4
Blackburn GL, Bistrian BR, Maini BS, Schlamm HT, Smith MF (1977) Nutritional and metabolic assessment of the hospitalized patient. JPEN J Parenter Enteral Nutr 1:11–22
Bowman BB, Rosenberg IH (1982) Assessment of the nutritional status of the elderly. Am J Clin Nutr 35:1142–1151
Brennan MF (1977) Uncomplicated starvation versus cancer cachexia. Cancer Res 37:2359–2364
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr (1999) Body-mass index and mortality in a prospective cohort of U.S. adults [see comments]. N Engl J Med 341:1097–1105
Cleveland Clinic Foundation (1999) Guide to laboratory services. Pathology and Laboratory Medicine. The Cleveland Clinic Foundation, Cleveland, OH
Cohn SH, Gartenhaus W, Sawitsky A, et al (1981) Compartmental body composition of cancer patients by measurement of total body nitrogen, potassium, and water. Metabolism 30:222–229
Cohn SH, Gartenhaus W, Vartsky D, et al (1981) Body composition and dietary intake in neoplastic disease. Am J Clin Nutr 34:1997–2004
Delmore G (1997) Assessment of nutritional status in cancer patients: widely neglected? Support Care Cancer 5:376–380
Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, Jeejeebhoy KN (1984) Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enteral Nutr 8:153–159
Donnelly S, Walsh D, Rybicki L (1995) The symptoms of advanced cancer: identification of clinical and research priorities by assessment of prevalence and severity. J Palliat Care 11:27–32
Edwards BK, Howe HL, Ries LA, et al (2002) Annual report to the nation on the status of cancer, 1973–1999, featuring implications of age and aging on U.S. cancer burden. Cancer 94:2766–2792
Falconer JS, Fearon KC, Plester CE, Ross JA, Carter DC (1994) Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann Surg 219:325–331
Forbes GB, Brown MR, Griffiths HJ (1988) Arm muscle plus bone area: anthropometry and CAT scan compared. Am J Clin Nutr 47:929–931
Freeman LM, Roubenoff R (1994) The nutrition implications of cardiac cachexia. Nutr Rev 52:340–347
Frisancho AR (1974) Triceps skin fold and upper arm muscle size norms for assessment of nutrition status. Am J Clin Nutr 27:1052–1058
Frisancho AR (1981) New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr 34:2540–2545
Frisancho AR (1984) New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am J Clin Nutr 40:808–819
Frisancho AR (1988) Nutritional anthropometry. J Am Diet Assoc 88:553–555
Goodinson SM (1987) Assessment of nutritional status. Prof Nurse 2:367–369
Goulet O (1998) Assessment of nutritional status in clinical practice. Baillieres Clin Gastroenterol 12:647–669
Harris J, Benedict F (1919) A biometric study of basal metabolism in man. Carnegie Institute of Washington, Washington, DC
Heiat A, Vaccarino V, Krumholz HM (2001) An evidence-based assessment of federal guidelines for overweight and obesity as they apply to elderly persons. Arch Intern Med 161:1194–1203
Heymsfield SB, McManus CB (1985) Tissue components of weight loss in cancer patients. A new method of study and preliminary observations. Cancer 55:238–249
Heymsfield SB, McManus C, Smith J, Stevens V, Nixon DW (1982) Anthropometric measurement of muscle mass: revised equations for calculating bone-free arm muscle area. Am J Clin Nutr 36:680–690
Hirsch S, de Obaldia N, Petermann M, et al (1991) Subjective global assessment of nutritional status: further validation. Nutrition 7:35–37
Jeejeebhoy KN, Meguid MM (1986) Assessment of nutritional status in the oncologic patient. Surg Clin North Am 66:1077–1090
Jeejeebhoy KN, Detsky AS, Baker JP (1990) Assessment of nutritional status. JPEN J Parenter Enteral Nutr 14:193S–196S
Komurcu S, Nelson K, Walsh D, Ford R, Rybicki L (2002) Gastrointestinal symptoms amongst inpatients with advanced cancer. Am J Hosp Palliat Care 19:351–355
Kotler DP (2000) Cachexia. Ann Intern Med 133:622–634
Kushner RF (1992) Bioelectrical impedance analysis: a review of principles and applications. J Am Coll Nutr 11:199–209
Lawson DH, Richmond A, Nixon DW, Rudman D (1982) Metabolic approaches to cancer cachexia. Annu Rev Nutr 2:277–301
Lipkin EW, Bell S (1993) Assessment of nutritional status. The clinician's perspective. Clin Lab Med 13:329–352
Lolli R, Marchesini G, Bianchi G, et al (1992) Anthropometric assessment of the nutritional status of patients with liver cirrhosis in an Italian population. Ital J Gastroenterol 24:429–435
Lukaski HC (1987) Methods for the assessment of human body composition: traditional and new. Am J Clin Nutr 46:537–556
Lukaski HC, Bolonchuk WW, Hall CB, Siders WA (1986) Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol 60:1327–1332
Merli M, Riggio O, Romiti A, et al (1990) Basal energy production rate and substrate use in stable cirrhotic patients. Hepatology 12:106–112
Mullen JL, Gertner MH, Buzby GP, Goodhart GL, Rosato EF (1979) Implications of malnutrition in the surgical patient. Arch Surg 114:121–125
Neale G (1990) Undernutrition. Med Int 82:3386–3391
Nelson KA (2000) The cancer anorexia-cachexia syndrome. Semin Oncol 27:64–68
Nelson KA, Walsh D, Sheehan FA (1994). The cancer anorexia-cachexia syndrome [see comments]. J Clin Oncol 12:213–225
Ottery FD (1994) Rethinking nutritional support of the cancer patient: the new field of nutritional oncology. Semin Oncol 21:770–778
Ottery FD (1995) Supportive nutrition to prevent cachexia and improve quality of life. Semin Oncol 22:98–111
Ottery FD (1996) Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 12:S15–S19
Paijmans IJ, Wilmore KM, Wilmore JH (1992) Use of skinfolds and bioelectrical impedance for body composition assessment after weight reduction. J Am Coll Nutr 11:145–151
Smith LC, Mullen JL (1991) Nutritional assessment and indications for nutritional support. Surg Clin North Am 71:449–457
Staal-van den Brekel AJ, Schols AM, ten Velde GP, Buurman WA, Wouters EF (1994) Analysis of the energy balance in lung cancer patients 1. Cancer Res 54:6430–6433
Tisdale MJ (2001) Cancer anorexia and cachexia. Nutrition 17:438–442
Van Loan M, Mayclin P (1987) Bioelectrical impedance analysis: is it a reliable estimator of lean body mass and total body water. Hum Biol 59:299–309
Warren S (1932) The immediate causes of death in cancer. Am J Med Sci 184:610–615
Wigmore SJ, Falconer JS, Plester CE, et al (1995) Ibuprofen reduces energy expenditure and acute-phase protein production compared with placebo in pancreatic cancer patients. Br J Cancer 72:185–188
World Health Organization (2000) Obesity: preventing and managing the global epidemic (Technical Report Series, no. 894). WHO, Geneva
Xing Z, Gauldie J, Cox G, et al (1998) IL-6 is an anti-inflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest 101:311–320
Author information
Authors and Affiliations
Corresponding author
Additional information
The Harry R. Horvitz Center for Palliative Medicine is a World Health Organization Demonstration Project in Palliative Medicine.
This work was presented at the American Society of Clinical Oncology 35th Annual Meeting in Atlanta, Georgia, May 15–18, 1999.
Rights and permissions
About this article
Cite this article
Sarhill, N., Mahmoud, F., Walsh, D. et al. Evaluation of nutritional status in advanced metastatic cancer. Support Care Cancer 11, 652–659 (2003). https://doi.org/10.1007/s00520-003-0486-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-003-0486-0