Summary
Background
Inadequate nutritional status has been linked to poor outcomes in patients with heart failure (HF). Skeletal muscle wasting affects about 20% of ambulatory patients with HF. The impact of nutritional intake and appetite on skeletal muscle wasting has not been investigated so far. We sought to investigate the impact of nutritional status on muscle wasting and mortality in ambulatory patients with HF.
Methods
We studied 130 ambulatory patients with HF who were recruited as a part of the Studies Investigating Co-morbidities Aggravating Heart Failure (SICA-HF) program. Muscle wasting was defined according to criteria of sarcopenia, i.e., appendicular skeletal muscle mass two standard deviations below the mean of a healthy reference group aged 18–40 years. Nutritional status was evaluated using the Mini-Nutritional Assessment—Short Form (MNA-SF). Functional capacity was assessed as peak oxygen consumption (peak VO2) by cardiopulmonary exercise testing, 6‑minute walk testing, and the Short Physical Performance Battery (SPPB).
Results
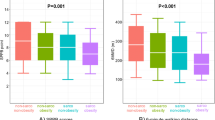
At baseline, 19 patients (15%) presented with muscle wasting. Patients with muscle wasting had significantly lower values of peak VO2, 6‑minute walk distance, SPPB, and MNA-SF score than patients without (all p < 0.05). In multivariate analysis, MNA-SF remained an independent predictor of muscle wasting after adjustment for age and New York Heart Association class (odds ratio [OR] 0.66; confidence interval [CI] 0.50–0.88; p < 0.01). A total of 16 (12%) patients died during a mean follow-up of 21 months. In Cox regression analysis, MNA-SF (OR 0.80, CI 0.64–0.99, p = 0.04), left ventricular ejection fraction (OR 0.93, CI 0.86–0.99, p = 0.05), and peak VO2 (OR 0.78, CI 0.65–0.94, p = 0.008) were predictors of death.
Conclusion
MNA-SF is an independent predictor of muscle wasting and mortality in ambulatory patients with HF. Nutritional screening should be included as a fundamental part of the overall assessment of these patients.




Similar content being viewed by others
References
Grande AJ, Silva V, Maddocks M. Exercise for cancer cachexia in adults: executive summary of a Cochrane collaboration systematic review. J Cachexia Sarcopenia Muscle. 2015;6:208–11.
Koca I, Savas E, Ozturk ZA, et al. The evaluation in terms of sarcopenia of patients with fibromyalgia syndrome. Wien Klin Wochenschr. 2015; doi:10.1007/s00508-015-0821-8.
Jones SE, Maddocks M, Kon SS, Canavan JL, Nolan CM, Clark AL, et al. Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax. 2015;70:213–8.
Foley RN, Wang C, Ishani A, Collins AJ, Murray AM. Kidney function and sarcopenia in the United States general population: NHANES III. Am J Nephrol. 2007;27:279–86.
Fülster S, Tacke M, Sandek A, Ebner N, Tschöpe C, Doehner W, et al. Muscle wasting in patients with chronic heart failure: results from the studies investigating co-morbidities aggravating heart failure (SICA-HF). Eur Heart J. 2013;34:512–9.
Bekfani T, Pellicori P, Morris DA, Ebner N, Valentova M, Steinbeck L, et al. Sarcopenia in patients with heart failure with preserved ejection fraction: Impact on muscle strength, exercise capacity and quality of life. Int J Cardiol. 2016;222:41–6.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200. doi:10.1093/eurheartj/ehw128..
Kim KM, Lim S, Choi SH, Kim JH, Shin CS, Park KS, et al. Cardiometabolic implication of sarcopenia: The Korea National Health and Nutrition Examination Study (KNHANES) 2008–2010. IJC Metab Endocr. 2014;4:63–9.
Segura A, Pardo J, Jara C, Zugazabeitia L, Carulla J, de Las Peñas R, et al. An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin Nutr. 2005;24:801–14.
Konishi M, Ishida J, von Haehling S, et al. Nutrition in cachexia: from bench to bedside. J Cachexia Sarcopenia Muscle. 2016; doi:10.1002/jcsm.12111.
Sandek A, Do Bowenehner W, Anker SD, von Haehling S. Nutrition in heart failure: an update. Curr Opin Clin Nutr Metab Care. 2009;12:384–91.
Tacke M, Ebner N, Boschmann M, Jarius A, Valentova M, Fulster S, et al. Resting energy expenditure and the effects of muscle wasting in patients with chronic heart failure: results from the Studies Investigating Comorbidities Aggravating Heart Failure (SICA-HF). J Am Med Dir Assoc. 2013;14:837–41.
Anker SD, Coats AJ. Cardiac cachexia: a syndrome with impaired survival and immune and neuroendocrine activation. Chest. 1999;115:836–47.
Elia M. The “MUST” Report. Nutritional Screening of Adults: A Multidisciplinary Responsibility. Redditch, UK: British Association for Parenteral and Enteral Nutrition 2003. http://www.bapen.org.uk/pdfs/must/must_exec_sum.pdf. Accessed 31.06.2016.
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z. Ad Hoc ESPEN Working Group. Nutritional Risk Screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22:321–36.
Lainscak M, Farkas J, Frantal S, et al. Self-rated health, nutritional intake and mortality in adult hospitalized patients. Eur J Clin Invest. 2014;44(9):813–24.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN guidelines for nutritional screening 200. Clin Nutr. 2003;22:415–21.
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F, Bennahum D, Lauque S, et al. The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition. 1999;15:116–22.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form Mini-Nutritional Assessment (MNA-SF). J Gerontol A Biol Sci Med Sci. 2001;56:M366–372.
Guerra-Sánchez L, Martínez-Rincón C, Fresno-Flores M. Nutritional screening in heart failure patients: 5 methods review. Nutr Hosp. 2014;31(2):890–9.
Sargento L, Satendra M, Almeida I, Sousa C, Gomes S, Salazar F, et al. Nutritional status of geriatric outpatients with systolic heart failure and its prognostic value regarding death or hospitalization, biomarkers and quality of life. J Nutr Health Aging. 2013;17:300–4.
Bonilla-Palomas JL, Gámez-López AL, Anguita-Sánchez MP, Castillo-Domínguez JC, García-Fuertes D, Crespin-Crespin M, et al. Impact of malnutrition on long-term mortality in hospitalized patients with heart failure. Rev Esp Cardiol. 2011;64:752–8.
von Haehling S, Lainscak M, Doehner W, Ponikowski P, Rosano G, Jordan J, et al. Diabetes mellitus, cachexia and obesity in heart failure: rationale and design of the Studies Investigating Co-morbidities Aggravating Heart Failure (SICA-HF). J Cachexia Sarcopenia Muscle. 2010;1:187–94.
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–63.
Heymsfield SB, Smith R, Aulet M, Bensen B, Lichtman S, Wang J, et al. Appendicular skeletal muscle mass: measurement by dual-photon absorptiometry. Am J Clin Nutr. 1990;52:214–8.
Morley JE, Baumgartner RN, Roubenoff R, Mayer J, Nair KS. Sarcopenia. J Lab Clin Med. 2001;137:231–43.
Guralnik JM, Simonsick EM, Ferrucci L. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332(9):556–61.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Hasselmann M, Alix E. Tools and procedures for screening for malnutrition and its associated in risks in hospital. Nutr Clin Metabol. 2003;17:218–26.
von Haehling S. The wasting continuum in heart failure: from sarcopenia to cachexia. Proc Nutr Soc. 2015;74(4):367–77.
Loncar G, Bozic B, von Haehling S, Düngen HD, Prodanovic N, Lainscak M, et al. Association of adiponectin with peripheral muscle status in elderly patients with heart failure. Eur J Intern Med. 2013;24(8):818–23.
von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle. 2010;1:129–33.
Morley JE, von Haehling S, Anker SD, et al. From sarcopenia to frailty: a road less traveled. J Cachexia Sarcopenia Muscle. 2014;5(1):5–8.
Mitch WE. Malnutrition is an unusual cause of decreased muscle mass in chronic kidney disease. J Ren Nutr. 2007;17:66–9.
Langen RC, Gosker HR, Remels AH, Schols AM. Triggers and mechanisms of skeletal muscle wasting in chronic obstructive pulmonary disease. Int J Biochem Cell Biol. 2013;45:2245–56.
von Haehling S, Steinbeck L, Doehner W, Springer J, Anker SD. Muscle wasting in heart failure: An overview. Int J Biochem Cell Biol. 2013;45(10):2257–65.
Horwich TB, Kalantar-Zadeh K, MacLellan RW, Fonarow GC. Albumin levels predict survival in patients with systolic heart failure. Am Heart J. 2008;155(5):883–9.
Doweiko JP, Nompleggi DJ. The role of albumin in human physiology and patho-physiology, Part III: Albumin and disease states. JPEN J Parenter Enteral Nutr. 1991;15(4):476–83.
Aziz EF, Javed F, Pratap B, Musat D, Nader A, Pulimi S, et al. Malnutrition as assessed by nutritional risk index is associated with worse outcome in patients admitted with acute decompensated heart failure: an ACAP-HF data analysis. Heart Int. 2011;6(1):e2.
Omran ML, Morley JE. Assessment of protein energy malnutrition in older persons, part I: History, examination, body composition, and screening tools. Nutrition. 2000;16:50–63.
Htun NC, Ishikawa-Takata K, Kuroda A, Tanaka T, Kikutani T, Obuchi SP, et al. Screening for Malnutrition in Community Dwelling Older Japanese: Preliminary Development and Evaluation of the Japanese Nutritional Risk Screening Tool (NRST). J Nutr Health Aging. 2016;20(2):114–20.
Hirose T, Hasegawa J, Izawa S, Enoki H, Suzuki Y, Kuzuya M. Accumulation of geriatric conditions is associated with poor nutritional status in dependent older people living in the community and in nursing homes. Geriatr Gerontol Int. 2014;14:198–205.
Steinbeck L, Ebner N, Valentova M, Bekfani T, Elsner S, Dahinden P, et al. Detection of muscle wasting in patients with chronic heart failure using C‑terminal agrin fragment: results from the Studies Investigating Co-morbidities Aggravating Heart Failure (SICA-HF). Eur J Heart Fail. 2015;17(12):1283–93.
Yost G, Gregory M, Bhat G. Short-form nutrition assessment in patients with advanced heart failure evaluated for ventricular assist device placement or cardiac transplantation. Nutr Clin Pract. 2014;29(5):686–91.
Arena R, Myers J, Guazzi M. The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence- based review. Heart Fail Rev. 2008;13:245–69.
Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH Jr, Wilson JR. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation. 1991;83:778–86.
Azhar G, Wei JY. Nutrition and cardiac cachexia. Curr Opin Clin Nutr Metab Care. 2006;9:18–23.
Lenk K, Erbs S, Höllriegel R, Beck E, Linke A, Gielen S, et al. Exercise training leads to a reduction of elevated myostatin levels in patients with chronic heart failure. Eur J Prev Cardiol. 2012;19:404–11.
Smart NA, Steele M. The effect of physical training on systemic proinflammatory cytokine expression in heart failure patients: a systematic review. Congest Heart Fail. 2011;17:110–4.
Bowen TS, Schuler G, Adams V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachexia Sarcopenia Muscle. 2015;6(3):197–207.
Cebron Lipovec N, Schols AM, van den Borst B, et al. Sarcopenia in advanced COPD affects cardiometabolic risk reduction by short-term high-intensity pulmonary rehabilitation. J Am Med Dir Assoc. 2016;17(9):814–20.
Vonbank K, Zwick RH, Strauss M, et al. Guidelines for outpatient pulmonary rehabilitation in Austria. Wien Klin Wochenschr. 2015;127(13–14):503–13.
Fearon K, Argiles JM, Baracos VE, et al. Request for regulatory guidance for cancer cachexia intervention trials. J Cachexia Sarcopenia Muscle. 2015;6(4):272–4.
van Deursen VM, Urso R, Laroche C, Damman K, Dahlström U, Tavazzi L, et al. Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16(1):103–11.
Hummel SL, Herald J, Alpert C, Gretebeck KA, Champoux WS, Dengel DR, et al. Submaximal oxygen uptake kinetics, functional mobility, and physical activity in older adults with heart failure and reduced ejection fraction. J Geriatr Cardiol. 2016;13(5):450–7.
Funding
This project was supported by the 7th framework program (FP7/2007/2013) under grant agreement number 241558 of the European Commission (SICA-HF). M.R.S. was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq 234052/2014-7). Part of the present work was additionally funded by a grant from the Innovative Medicines Initiative—Joint Undertaking (IMI–JU 115621, SPRINT-T).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Saitoh, M.R. dos Santos, N. Ebner, A. Emami, M. Konishi, J. Ishida, M. Valentova, A. Sandek, W. Doehner, S.D. Anker, and S. von Haehling declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Saitoh, M., dos Santos, M.R., Ebner, N. et al. Nutritional status and its effects on muscle wasting in patients with chronic heart failure: insights from Studies Investigating Co-morbidities Aggravating Heart Failure. Wien Klin Wochenschr 128 (Suppl 7), 497–504 (2016). https://doi.org/10.1007/s00508-016-1112-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-016-1112-8