Summary
Objectives
Inflammatory bowel disease (IBD) in children has a remitting and relapsing course. The aim of our study was to evaluate the value of fecal calprotectin (FC), C-reactive protein (CRP), and clinical scores in predicting endoscopic and histological lesions in children with IBD.
Methods
A total of 68 children with IBD (29 with ulcerative colitis (UC), 39 with Crohn’s disease (CD), mean age 14.2 years) were included in the study.
We retrospectively reviewed clinical scores (PUCAI, PCDAI), CRP values, endoscopic, and histological data as well as FC values in all included children.
Results
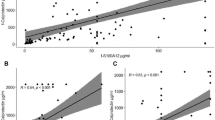
In children with UC, the correlation between the histological lesions and FC (r = 0.609, p < 0.01), CRP (r = 0.390, n.s.), or PUCAI (r = 0.535, p < 0.05) was higher than for children with CD (FC r = 0.490, n.s.; CRP r = 0.269, n.s.; PCDAI r = 0.257, n.s.). The correlation between endoscopy scores and the same parameters yielded similar findings (UC: FC r = 0.628, p < 0.01; CRP r = 0.387, n.s.; PUCAI r = 0.256, n.s.; CD: FC r = 0.516, p < 0.05; CRP r = 0.238, n.s.; PCDAI r = 0.267, n.s.).
The correlation between FC and PUCAI (r = 0.532, p < 0.01) was higher than that between CRP and PUCAI (r = 0.424, p < 0.01). However, the correlation between FC and PCDAI (0.384, p < 0.01) is lower than that between CRP and PCDAI (r = 0.447, p < 0.01).
Conclusion
FC is a better predictor of the severity of endoscopic and histological lesions than CRP or disease activity scores, especially for UC. FC, as a noninvasive marker, could possibly be used to reduce the number of endoscopic procedures in children with a confirmed diagnosis of IBD.



Similar content being viewed by others
References
Konikoff MR, Denson LA. Role of fecal calprotectin as a biomarker of intestinal inflammation in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12:524–34.
Jelsness-Jørgensen LP, Bernklev T, Moum B. Calprotectin is a useful tool in distinguishing coexisting irritable bowel like symptoms from that of occult inflammation among inflammatory bowel disease patients in remission. Gastroenterol Res Pract. 2013;2013:620707.
Aomatsu T, Yodel A, Matsumoto K, et al. Fecal calprotectin is a useful marker for disease activity in pediatric patients with inflammatory bowel disease. Dig Dis Sci. 2011;56:2372–7.
García-Sánches V, Iglesias-Flores E, Gonzáles R, et al. Does fecal calprotectin predict relapse in patients with Crohn’s disease and ulcerative colitis. J Crohns Colitis. 2010;4:144–52.
Levine A, Koletzko S, Turner D, et al. The ESPHGAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795–806.
Komraus M, Wos H, Wiecek S, et al. Usefulness of faecal calprotectin measurement in children with various types of inflammatory bowel disease. Mediators Inflamm. 2012;2012:608249.
Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis. 2014;8:1179–207.
Turner D, Levine A, Escher JC, et al. Management of pediatric ulcerative colitis: joint ECCO and ESPGHAN evidence-based consensus guidelines. J Pediatr Gastroenterol Nutr. 2012;55:340–61.
Sandhu BK, Fell JM, Beattie RM, et al. Guidelines for the management of inflammatory bowel disease in children in the United Kingdom. J Pediatr Gastroenterol Nutr. 2010;50:S1–13.
Henderson P, Anderson NH, Wilson DC. The diagnostic accuracy of fecal calprotecin during the investigation of suspected pediatric inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol. 2014;109:637–45.
Henderson P, Casey A, Lawrence SJ, et al. The diagnostic accuracy of fecal calprotectin during the investigation of suspected pediatric inflammatory bowel disease. Am J Gastroenterol. 2012;107:941–9.
Fagerberg Lorentzon U, Lööf L, Lindholm J, et al. Fecal calprotectin: a quantitative marker of colonic inflammation in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2007;45:414–20.
Bunn SK, Bisset WM, Main MJC, et al. Fecal calprotectin as a measure of disease activity in childhood inflammatory bowel disease. J Pediatr Gstroenterol Nutr. 2001;32:171–7.
Canani RB, Terrin G, Rapacciuolo L, et al. Faecal calprotectin as reliable non-invasive marker to assess the severity of mucosal inflammation in children with inflammatory bowel disease. Dig Liver Dis. 2008;40:547–53.
Hyams JS, Ferry GD, Mandel FS, et al. Developement and validation of a Pediatric Crohn’s Disease Activity Index. J Pediatr Gastroenterol Nutr. 1991;12:439–47.
Turner D, Oatley D, Mack D, et al. Developement, validation and evaluation of pediatric ulcerative colitis activity index: a prospective multicentric study. Gastroenterology. 2007;133:423–32.
Quail MA, Russell RK, Van Limbergen JE, et al. Fecal calprotectin complements routine laboratory investigations in diagnosing childhood inflammatory bowel disease. Inflamm Bowel Dis. 2009;15:756–9.
Bremner A, Roked S, Robinson R, et al. Faecal calprotectin in children with chronic gastrointestinal symptoms. Acta Paediatr. 2005;94:1855–8.
Gisbert JP, McNicholl AG. Questions and answers on the role of fecal calprotectin as a biological marker of inflammatory bowel disease. Dig Liver Dis. 2009;41:56–66.
Montalto M, Gallo A, Santoro L, et al. Role of fecal calprotectin in gastrointestinal disorders. Eur Rev Med Pharmacol Sci. 2013;17:1569–82.
Degraeuwe P, Beld M, Ashorn M, et al. Faecal calprotectin in suspected paediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2015;60:339–46.
Sidler MA, Leach ST, Day AS. Fecal S100A12 and fecal calprotectin as noninvasive markers for inflammatory bowel disease in children. Inflamm Bowel Dis. 2008;14:359–66.
Bunn SK, Bisset WM, Main MJ, et al. Fecal calprotectin: validation as a noninvasive measure of bowel inflammation in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2001;33:14–22.
Diamanti A, Colistro F, Basso MS, et al. Clinical role of calprotectin assay in determining histological relapses in children affected by inflammatory bowel diseases. Inflamm Bowel Dis. 2008;14:1229–35.
Olafsdottir E, Aksnes L, Fluge G, et al. Faecal calprotectin levels in infants with infantile colic, healthy infants, children with inflammatory bowel disease, children with recurrent abdominal pain and healthy children. Acta Paediatr. 2002;91:45–50.
Önal I, Beyazit Y, Şener B, Savuk B, Özer Etik D, Sayilir A, et al. The value of fecal carprotectin as a marker of intestinal inflammation in patients with ulcerative colitis. Turk J Gastroenterol. 2012;23(5):509–14.
D’Haens G, Ferrante M, Vermeire S, Baert F, Noman M, Moortgat L, et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis. 2012;18:2218–24.
Kolho KL, Sipponen T, Valtonen E, Savilathi E. Fecal calprotectin, MMP-9, and human beta-defensin-2 levels in pediatric inflammatory bowel disease. Int J Colorectal Dis. 2014;29:43–50.
Berni Canani R, Rapacciuolo L, Romano MT, et al. Diagnostic value of faecal calprotectin in paediatric gastroenterology clinical practice. Dig Liver Dis. 2004;36:467–70.
Kolho KL, Turner D. Fecal calprotectin and clinical disease activity in pediatric ulcerative colitis. ISRN Gastroenterol. 2013;2013:179024.
Acknowledgments
The authors wish to thank all the children and their parents whose data was included in the study. We are also grateful to the medical personnel of the Gastroenterology Unit, Department of Pediatrics, University Medical Center Maribor, Slovenia.
Conflict of interest
Jernej Dolinsek, MD, PhD, Larisa Sabath, Petra Riznik, MD and Dusanka Micetic-Turk, MD, PhD, declare that there are no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dolinšek, J., Rižnik, P., Sabath, L. et al. Fecal calprotectin as a marker of the severity of mucosal inflammation in children with inflammatory bowel disease. Wien Klin Wochenschr 128, 253–259 (2016). https://doi.org/10.1007/s00508-015-0915-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-015-0915-3