Summary
Background
Late-onset infections are an important cause of morbidity and mortality in preterm infants. The purpose of our prospective randomised study was to establish whether a combination of probiotics (Lactobacillus acidophilus, Enterococcus faecium and Bifidobacterium infantum) affects the incidence of late-onset sepsis and other infections in very low birthweight infants (birthweight under 1500 g, gestational age under 33 weeks).
Methods
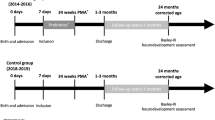
From 80 included infants, one half received probiotics (L. acidophilus, E. faecium and B. infantum) in the ratio 1.5:1:1.5, at a dose of 0.6 × 107 colony-forming units twice daily, given with the first portions of milk until discharge, whereas the other half did not.
Results
In the group receiving probiotics, 16 children had late-onset sepsis compared with 29 in the group without probiotics; p = 0.006. The number of late-onset septic events was lower (30) in the group receiving probiotics than in the group that did not receive probiotics (69); p = 0.003. Furthermore, fewer children had at least one late-onset infection (20 infants in the group receiving probiotics compared with 32 in the group without them; p = 0.009). There were less episodes of late-onset infections in the group receiving probiotics (35) than in the group without probiotics (79); p = 0.002.
Conclusions
A combination of probiotics at a low dose (1.2 × 107 colony-forming units) decreased the frequency of late-onset sepsis and other infections, as described in previous studies. In addition, children were discharged at a lower postmenstrual age. There were no side effects of probiotics reported.

Similar content being viewed by others
References
Awad H, Mokhtar H, Imam SS, Gad GI, Hafez H, Aboushady N. Comparison between killed and living probiotic usage versus placebo for the prevention of necrotizing enterocolitis and sepsis in neonates. Pak J Biol Sci. 2010;13(6):253–62.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Ann Surg. 1978;187(1):1–7.
Bezirtzoglou E, Tsiotsias A, Welling GW. Microbiota profile in feces of breast- and formula-fed newborns by using fluorescence in situ hybridization (FISH). Anaerobe. 2011;17(6):478–82.
Bianconi S, Gudavalli M, Sutija VG, Lopez AL, Barillas-Arias L, Ron N. Ranitidine and late-onset sepsis in the neonatal intensive care unit. J Perinat Med. 2007;35(2):147–50.
Bradley JS. Considerations unique to pediatrics for clinical trial design in hospital acquired pneumonia and ventilator assiciated pneumonia. Clin Infect Dis. 2010;51(S1):136–43.
Burja S, Treiber M, Tekauc-Golob A, et al. Neonatal mortality in the Maribor region (1997–2008). Acta medico-biotechnica. 2014;7(1):23–31.
Carl MA, Ndao IM, Springman AC, Manning SD, Johnson JR, Johnson BD, et al. Sepsis from the gut: the enteric habitat of bacteria that cause late-onset neonatal bloodstream infections. Clin Infect Dis. 2014;58(9):1211–8.
Cheng YW, Wong SN. Diagnosing symptomatic urinary tract infections in infants by catheter urine culture. J Paediatr Child Health. 2005;41:437–40.
Costalos C, Skouteri V, Gounaris A, Sevastiadou S, Triandafilidou A, Ekonomidou C, et al. Enteral feeding of premature infants with Saccharomyces boulardii. Early Hum Dev. 2003;74(2):89–96.
Dani C, Biadaioli R, Bertini G, Martelli E, Rubaltelli FF. Probiotics feeding in prevention of urinary tract infection, bacterial sepsis and necrotizing enterocolitis in preterm infants. A prospective double-blind study. Biol Neonate. 2002;82(2):103–8.
Duffy LC. Interactions mediating bacterial translocation in the immature intestine. J Nutr. 2000;130(2S Suppl):432S–6S.
Ehrenkrantz RA. Early, aggressive nutritional management for very low birth weight infants: what is the evidence? Semin Perinatol. 2007;31(2):48–55.
Fernandez-Carrocera LA, Solis-Herrera A, Cabanillas-Ayon M, Gallardo-Sarmiento RB, Garcia-Perez CS, Montano-Rodriguez R, et al. Double-blind, randomised clinical assay to evaluate the efficacy of probiotics in preterm newborns weighing less than 1500 g in the prevention of necrotising enterocolitis. Arch Dis Child Fetal Neonatal Ed. 2013;98:F5–9.
Gill HS. Probiotics enhance anti-effective defences in the gastrointestinal tract. Best Pract Res Clin Gastroenterol. 2003;17(5):755–73.
Gray JW. Which factors predict hospital-acquired late-onset neonatal sepsis? Pediatr Health. 2008;2(4):477–84.
Kaufman D, Fairchild KD. Clinical microbiology of bacterial and fungal sepsis in very-low-birth-weight infants. Clin Microbiol Rev. 2004;17(3):638–80.
Kolaček S. Imunost probavnog sustava. Paediatr Croat. 2005;49(Suppl. 1):89–93.
Lin HC, Su BH, Chen AC, Lin TW, Tsai CH, Yeh TF, et al. Oral probiotics reduce the incidence and severity of necrotizing enterocolitis in very low birth weight infants. Pediatrics. 2005;115(1):1–4.
Lin HC, Hsu CH, Chen HL, Chung MY, Hsu JF, Lien RI, et al. Oral probiotics prevent necrotizing enterocolitis in very low birth weight preterm infants: a multicenter, randomized, controlled trial. Pediatrics. 2008;122(4):693–700.
Melvan JN, Bagby GJ, Welsh DA, Nelson S, Zhang P. Neonatal sepsis and neutrophil insufficiencies. Int Rev Immunol. 2010;29(3):315–48.
Mičetić-Turk D, Šikić-Pogačar M. Klinična uporaba probiotikov v pediatriji. Zdrav Vestn. 2011;80:933–43.
Mihatsch WA, von Schoenaich P, Fahnenstich H, et al. The significance of gastric residuals early enteral feeding advancement of extremely low birth weight infants. Pediatrics. 2002;109(3):457–9.
Mihatsch WA, Vossbeck S, Eikmanns B, Hoegel J, Pohlandt F. Effect of bifidobacterium lactis on the incidence of nosocomial infections in very-low-birthweight infants: a randomized controlled trial. Neonatology. 2010;98(2):156–63.
Millar MR, Bacon C, Smith SL, Walker V, Hall MA. Enteral feeding of premature infants with Lactobacillus GG. Arch Dis Child. 1993;69(5):483–7.
Mohan R, Koebnick C, Schildt J, Mueller M, Radke M, Blaut M. Effects of Bifidobacterium lactis Bb12 supplementation on body weight, fecal pH, acetate, lactate, calprotectin, and IgA in preterm infants. Pediatr Res. 2008;64(4):418–22.
Neu J, Walker WA. Necrotising enterocolitis. N Engl J Med. 2011;354(3):255–64.
Palmer C, Bik EM, Digiulio DB, Relman DA, Brown PO. Development of the human infant intestinal microbiota. PLoS Biol. 2007;5(7):e177.
Philip AG, Mills PC. Use of C-reactive protein in minimizing antibiotic exposure: experience with infants initially admitted to a well-baby nursery. Pediatrics. 2000;106(1):E4.
Polin RA. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics. 2012;129(5):1006–15.
Polin RA, Denson S, Brady MT, Committee on Fetus and Newborn, Committee on Infectious Diseases. Epidemiology and diagnosis of health care-associated infections in the NICU. Pediatrics. 2012;129:e1104–9.
Robertson J, Shilkofski N. Chap. 25, Blood chemistry and body fluid. In: Robertson J, Shilkofski N, editors. The Harriet Lane handbook. 17th ed. Philadelphia: Mosby; 2005. pp. 661–72.
Samanta M, Sarkar M, Ghosh P, Ghosh J, Sinha M, Chatterjee S. Prophylactic probiotics for prevention of necrotizing enterocolitis in very low birth weight newborns. J Trop Pediatr. 2009;55(2):128–31.
Sawardekar KP. Changing spectrum of neonatal omphalitis. Pediatr Infect Dis J. 2004;23(1):22–6.
Shah BA, Padbury JF. Neonatal sepsis. An old problem with new insights. Virulence. 2014;5(1):170–8.
Stoll BJ, Hansen NI, Higgins RD, Fanaroff AA, Duara S, Goldberg R, et al. Very low birth weight preterm infants with early onset neonatal sepsis: the predominance of gram-negative infections continues in the National Institute of Child Health and Human Development Neonatal Research Network, 2002–2003. Pediatr Infect Dis J. 2005;24(7):635–9.
Tissiéres P. Innate immune deficiency of extremely premature neonates can be reversed by interferon-g. PLoS One. 2012;7:e32863.
Underwood MA, Salzman NH, Bennett SH, Barman M, Mills D, Marcobal A, et al. A randomized placebo-controlled comparison of two prebiotic/probiotic combinations in preterm infants: impact on weight gain, intestinal microbiota, and fecal short chain fatty acids. J Pediatr Gastroenterol Nutr. 2009;48(2):216–25.
US Food and Drug Administration Federal food, drug, and cosmetic act. 2004. http://www.fda.gov/opacom/laws/fdcact/fdcact4.htm. Accessed 12 May 2009.
Van der Zwet WC, Kaiser AM, van Elburg RM, Berkhof J, Fetterb WPF, Parlevlieta GA, Vandenbroucke-Graulsa CMJE. Nosocomial infections in a Dutch neonatal intensive care unit: surveillance study with definitions for infection specifically adapted for neonates. J Hosp Infect. 2005;61(4):300–11.
Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33(1):179–201.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kanic, Z., Micetic Turk, D., Burja, S. et al. Influence of a combination of probiotics on bacterial infections in very low birthweight newborns. Wien Klin Wochenschr 127 (Suppl 5), 210–215 (2015). https://doi.org/10.1007/s00508-015-0845-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-015-0845-0