Summary
Background
Prediction of the number of incident cancer cases is very relevant for health planning purposes and allocation of resources. The shift towards elder age groups in central European populations in the next decades is likely to contribute to an increase in cancer incidence for many cancer sites. In Tyrol, cancer incidence data have been registered on a high level of completeness for more than 20 years. We therefore aimed to compute well-founded predictions of cancer incidence for Tyrol for the year 2020 for all frequent cancer sites and for all cancer sites combined.
Methods
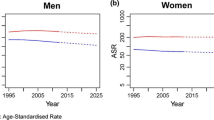
After defining a prediction base range for every cancer site, we extrapolated the age-specific time trends in the prediction base range following a linear model for increasing and a log-linear model for decreasing time trends. The extrapolated time trends were evaluated for the year 2020 applying population figures supplied by Statistics Austria.
Results
Compared with the number of annual incident cases for the year 2009 for all cancer sites combined except non-melanoma skin cancer, we predicted an increase of 235 (15 %) and 362 (21 %) for females and males, respectively. For both sexes, more than 90 % of the increase is attributable to the shift toward older age groups in the next decade. The biggest increase in absolute numbers is seen for females in breast cancer (92, 21 %), lung cancer (64, 52 %), colorectal cancer (40, 24 %), melanoma (38, 30 %) and the haematopoietic system (37, 35 %) and for males in prostate cancer (105, 25 %), colorectal cancer (91, 45 %), the haematopoietic system (71, 55 %), bladder cancer (69, 100 %) and melanoma (64, 52 %).
Conclusions
The increase in the number of incident cancer cases of 15 % in females and 21 % in males in the next decade is very relevant for planning purposes. However, external factors cause uncertainty in the prediction of some cancer sites (mainly prostate cancer and colorectal cancer) and the prediction intervals are still broad. Therefore, our predictions must be interpreted with some caution.
Zusammenfassung
Hintergrund
Die Vorhersage der Anzahl von inzidenten Krebspatienten für zukünftige Jahre ist sehr wichtig für die Gesundheitsplanung, insbesondere für die Planung von Ressourcen für den onkologischen Bereich. Allein die Verschiebung der Altersstruktur in Richtung ältere Jahrgänge wird in den nächsten Jahrzehnten zu einer Zunahme der inzidenten Krebsfälle für viele Krebsentitäten führen. In Tirol sammelt das Krebsregister Tirol die inzidenten Krebsfälle mit einem hohen Grad von Vollzähligkeit seit mehr als zwei Jahrzehnten. Daher war es unser Ziel, gut fundierte Vorhersagen für die Krebsinzidenz in Tirol für das Diagnosejahr 2020 zu berechnen, und zwar für die häufigen Krebsentitäten und für alle Krebsfälle zusammengefasst
Methoden
Nach der Definition eines Zeitraums für die Prognosebasis für jede einzelne Krebsentität haben wir die altersspezifischen Raten extrapoliert, und zwar mit einem linearen Modell bei einer Zunahme und mit einem loglinearen Modell bei einer Abnahme im Zeitraum für die Prognosebasis. Der extrapolierte Zeittrend wurde dann auf die Bevölkerungsstruktur von 2020 angewandt, die Bevölkerungszahlen wurden von der Statistik Austria prognostiziert.
Resultate
Verglichen mit den Anzahlen im Diagnosejahr 2009 wurde für die Zusammenfassung aller Krebsentitäten mit Ausnahme der nicht-melanotischen Hauttumore eine Zunahme von 235 (15 %) bei den Frauen und von 362 (21 %) bei den Männern prognostiziert. Für beide Geschlechter ist 90 % der Zunahme durch die Verschiebung der Altersstruktur erklärbar. Der stärkste Anstieg wurde bei den Frauen prognostiziert für Mammakarzinom (92, 21 %), Lungenkarzinom (64, 52 %), kolorektales Karzinom (40, 24 %), Melanom (38, 30 %) und Neubildungen im hämatopoetischen System (37, 35 %). Bei den Männern waren die stärksten Anstiege zu beobachten beim Prostatakarzinom (105, 25 %), kolorektalen Karzinom (91, 45 %), bösartigen Neubildungen im hämatopoetischen System (71, 55 %), Harnblasenkarzinom (69, 100 %) und Melanom (64, 52 %).
Schlussfolgerungen
Die Zunahme der Anzahl der neuerkrankten Krebsfälle von 15 % bei den Frauen und 21 % bei den Männern ist äußerst relevant für die Gesundheitsplanung. Allerdings verursachen externe Faktoren eine höheren Grad an Unsicherheit in der Vorhersage, insbesondere für Prostatakarzinome und kolorektale Karzinome, außerdem sind die Vorhersageintervalle breit. Daher müssen die Resultate mit Vorsicht interpretiert werden.



Similar content being viewed by others
Abbreviations
- NMSC:
-
Non-melanoma skin cancer
- PBR:
-
Prediction base range
- PCA:
-
Prostate cancer
- PSA:
-
Prostate-specific antigen
- BCA:
-
Breast cancer
References
Moller H, Fairley L, Coupland V, Okello C, Green M, Forman D, et al. The future burden of cancer in England: incidence and numbers of new patients in 2020. Br J Cancer. 2007 May 7;96(9):1484–8.
Curado MP, Edwards B, Shin H, Ferlay J, Heanue M, Boyle P, et al., editors. Cancer incidence in five continents. Volume IX. Lyon: IARC Sci Publ; 2008.
Oberaigner W, Siebert U. Are survival rates for Tyrol published in the Eurocare studies biased? Acta Oncol. 2009;48(7):984–84.
Dyba T, Hakulinen T, Paivarinta L. A simple non-linear model in incidence prediction. Stat Med. [Research Support, Non-U.S. Gov’t]. 1997 Oct 30;16(20):2297–309.
Dyba T, Hakulinen T. Do cancer predictions work? Eur J Cancer. [Research Support, Non-U.S. Gov’t]. 2008 Feb;44(3):448–53.
Hakulinen T, Dyba T. Precision of incidence predictions based on Poisson distributed observations. Stat Med. [Research Support, Non-U.S. Gov’t]. 1994 Aug 15;13(15):1513–23.
Stata Statistical Software: Release 11. College Station, Tx: StataCorp LP.2009.
Dyba T, Hakulinen T. Comparison of different approaches to incidence prediction based on simple interpolation techniques. Stat Med. [Comparative Study Research Support, Non-U.S. Gov’t Validation Studies]. 2000 Jul 15;19(13):1741–52.
Mikulasek A. Demographisches Jahrbuch 2011. Wien: Statistik Austria; 2012.
Bray F, Moller B. Predicting the future burden of cancer. NatRevCancer. 2006;6(1):63–74.
Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009 Jun 10;27(17):2758–65.
Pocobelli G, Cook LS, Brant R, Lee SS. Hepatocellular carcinoma incidence trends in Canada: analysis by birth cohort and period of diagnosis. Liver Int. [Research Support, Non-U.S. Gov’t]. 2008 Nov;28(9):1272–9.
Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. Lancet Oncol. 2012 Aug;13(8):790–801.
Lindemann K, Eskild A, Vatten LJ, Bray F. Endometrial cancer incidence trends in Norway during 1953–2007 and predictions for 2008–2027. Int J Cancer. [Comparative Study]. 2010 Dec 1;127(11):2661–8.
Amiri M, Janssen F, Kunst AE. The decline in stomach cancer mortality: exploration of future trends in seven European countries. Eur J Epidemiol. 2011 Jan;26(1):23–8.
Quon H, Loblaw A, Nam R. Dramatic increase in prostate cancer cases by 2021. BJU Int. 2011 Dec;108(11):1734–8.
Coupland VH, Okello C, Davies EA, Bray F, Moller H. The future burden of cancer in London compared with England. J Public Health (Oxf). [Comparative Study]. 2010 Mar;32(1):83–9.
Danaei G, Vander Hoorn S, Lopez AD, Murray CJ, Ezzati M. Causes of cancer in the world: comparative risk assessment of nine behavioural and environmental risk factors. Lancet. [Research Support, N.I.H., Extramural Research Support, U.S. Gov’t, P.H.S.]. 2005 Nov 19;366(9499):1784–93.
Strong K, Mathers C, Epping-Jordan J, Resnikoff S, Ullrich A. Preventing cancer through tobacco and infection control: how many lives can we save in the next 10 years? Eur J Cancer Prev. 2008 Apr;17(2):153–61.
Soerjomataram I, Barendregt JJ, Gartner C, Kunst A, Moller H, Avendano M. Reducing inequalities in lung cancer incidence through smoking policies. Lung Cancer. [Research Support, Non-U.S. Gov’t]. 2011 Sep;73(3):268–73.
Menvielle G, Soerjomataram I, de Vries E, Engholm G, Barendregt JJ, Coebergh JW, et al. Scenarios of future lung cancer incidence by educational level: modelling study in Denmark. Eur J Cancer. [Research Support, Non-U.S. Gov’t]. 2010 Sep;46(14):2625–32.
Didkowska J, Wojciechowska U, Koskinen HL, Tavilla A, Dyba T, Hakulinen T. Future lung cancer incidence in Poland and Finland based on forecasts on hypothetical changes in smoking habits. Acta Oncol. [Research Support, Non-U.S. Gov’t]. 2011 Jan;50(1):81–7.
Oberaigner W, Horninger W, Klocker H, Schonitzer D, Stuhlinger W, Bartsch G. Reduction of prostate cancer mortality in Tyrol, Austria, after introduction of prostate-specific antigen testing. Am J Epidemiol. 2006;164(4):376–84.
Oberaigner W, Siebert U, Horninger W, Klocker H, Bektic J, Schafer G, et al. Prostate-specific antigen testing in Tyrol, Austria: prostate cancer mortality reduction was supported by an update with mortality data up to 2008. Int J Public Health. 2012 Feb;57(1):57–62.
Bartsch G, Horninger W, Klocker H, Pelzer A, Bektic J, Oberaigner W, et al. Tyrol Prostate Cancer Demonstration Project: early detection, treatment, outcome, incidence and mortality. BJU Int. 2008 Apr;101(7):809–16.
Acknowledgements
We thank Patricia Gscheidlinger for her secretarial support, Lois Harrasser for assistance with statistical analyses and Mary Heaney Margreiter for native-speaker editing of the manuscript.
This work was supported by the ONCOTYROL Center for Personal Cancer Medicine. The Competence Center Oncotyrol is funded within the scope of the COMET—Competence Centers for Excellent Technologies through BMVIT, BMWFJ, through the province of Salzburg and the Tiroler Zukunftsstiftung/Standortagentur Tirol. The COMET Program is conducted by the Austrian Research Promotion Agency (FFG).
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oberaigner, W., Geiger-Gritsch, S. Prediction of cancer incidence in Tyrol/Austria for year of diagnosis 2020. Wien Klin Wochenschr 126, 642–649 (2014). https://doi.org/10.1007/s00508-014-0596-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0596-3