Summary
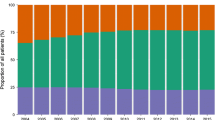
Diabetes Care Austria was a nationwide data acquisition of type 2 diabetes treatment at Austrian general practitioners. A total of 5,385 general practitioners were contacted in the end of 2009; finally, 101 agreed to participate in the data collection. Out of all 9 Austrian provinces, a cross-sectional sample of 1.513 type 2 diabetic patients was investigated. Demographic data, diabetes treatment, quality of diabetes control as well as micro- and macrovascular complications were analysed with respect to diabetes duration, categorised into 6 classes. A total of 1.513 type 2 diabetic patients with a mean age of 65.4 ± 10.7 years and a mean diabetes duration of 8.7 ± 7.3 years were analysed. Metformin was equally used in more than 50% of patients in all classes of diabetes duration. The use of sulfonylureas was significantly (p < 0.001) increased from 25% in patients with a diabetes duration of less than 3 years to more than 40% in subjects with a disease duration of longer than 15 years. The prescription of glitazones was significantly (p = 0.02) augmented with increasing diabetes duration. DPP-4 inhibitors were used in more than 5% of patients with a maximum of 13% in subjects with a diabetes duration of 4-9 years (p < 0.001). The mean HbA1c was below 7.5% in all classes and was significantly (p < 0.01) the lowest with 7.0 ± 1.2% in patients with the shortest diabetes duration when compared to all other categories. Diabetes Care Austria yielded representative data for diabetes therapy of type 2 diabetic patients treated by general practitioners. Diabetes treatment was successful, as proven by a mean HbA1c value of 7.2%. An insulin therapy was initialised late, but was nevertheless effective as shown by comparable HbA1c values in patients with a diabetes duration of 4 to more than 15 years.
Zusammenfassung
Diabetes Care Austria war eine Österreichweite Erhebung der Typ 2 Diabetestherapie bei niedergelassenen AllgemeinmedizinerInnen. Ende 2009 wurden 5.385 niedergelassene AllgemeinmedizinerInnen kontaktiert, von denen 101 an der Datenerhebung teilnahmen. Eine Querschnittstichprobe aus allen 9 österreichischen Bundesländern mit 1.513 Typ 2 DiabetikerInnen wurde untersucht. Neben demographischen Daten, Diabetestherapie und Qualität der Stoffwechselkontrolle wurden mikro- und makrovaskuläre Komplikationen in Abhängigkeit von der in 6 Klassen kategorisierten Diabetesdauer untersucht. Insgesamt wurden 1.513 Typ 2 Diabetiker mit einem mittleren Alter von 65,4 ± 10,7 Jahren und einer Diabetesdauer von 8,7 ± 7,3 Jahren erfasst. Metformin wurde in allen Kategorien der Diabetesdauer bei über 50 % der PatientInnen angewendet. Die Verwendung von Sulfonylharnstoffen nahm von 25 % bei einer Diabetesdauer von weniger als 3 Jahren auf über 40 % bei einer Diabetesdauer von mehr als 15 Jahren signifikant (p < 0,001) zu. Die Verschreibung von Glitazonen nahm signifikant (p = 0,02) mit der Diabetesdauer zu. DPP-4 Inhibitoren wurden bei über 5 % der Patienten (mit einem Häufigkeitsmaximum von 13 % bei einer Diabetesdauer von 4–9 Jahren, p < 0,001) eingesetzt Der mittlere HbA1c-Wert lag in allen Gruppen unter 7,5 % und war mit 7,0 ± 1,2 % in der Gruppe mit der kürzesten Diabetesdauer signifikant (p < 0,01) niedriger als in allen anderen Gruppen. Diabetes Care Austria ermöglicht repräsentative Daten bezüglich der Diabetestherapie für bei niedergelassenen AllgemeinmedizinerInnen behandelte Typ 2 DiabetikerInnen. Ein mittlerer HbA1c-Wert von 7,2 % belegt die erfolgreiche Diabetestherapie. Eine Insulintherapie wird relativ spät aber suffizient initiiert, wie vergleichbare HbA1c-Werte bei Patienten mit einer Diabetesdauer von 4 bis über 15 Jahren zeigen.
Similar content being viewed by others
Literatur
Hauner H, Koster I, von Ferber L. Prevalence of diabetes mellitus in Germany 1998–2001. Secondary data analysis of a health insurance sample of the AOK in Hesse/KV in Hessen. Dtsch Med Wochenschr 2003;128(50):2632–7
Dorner T, Rathmann T, Lechleitner M, Schlögel R, Roden M, Lawrence K, et al. Public health aspects of diabetes mellitus – epidemiology, prevention strategies, policy implications: the first Austrian diabetes report. Wien Klin Wochenschrift 2006;118(17–18):513–19
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352(9131):837–53
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Bmj 2000;321(7258):405–12
Diabetes mellitus–guidelines for the practice. Revised and expanded 2007 edition. Wien Klin Wochenschr 2009;121(Suppl. 5):S1–87
Davis TM, Davis Cyllene Uwa Edu Au WA, Bruce DG. Glycaemic levels triggering intensification of therapy in type 2 diabetes in the community: the Fremantle Diabetes Study. Med J Aust 2006;184(7):325–8
Macisaac RJ, Jerums G, Weekes AJ, Thomas MC. Patterns of glycaemic control in Australian primary care (NEFRON 8). Intern Med J 2009;39(8):512–8
Riddle MC, Rosenstock J, Gerich J. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26(11):3080–6
Raskin P, Allen E, Hollander P, et al. Initiating insulin therapy in type 2 Diabetes: a comparison of biphasic and basal insulin analogs. Diabetes Care 2005;28(2):260–5
Schiel R, Netzer C, Junghanel J, Muller UA. Metabolic control in patients with type-1 and type-2 diabetes mellitus receiving ambulatory care from general practitioners: results of a cross-sectional trial performed in the German federal states of Thuringia and West Pomerania. Z Evid Fortbild Qual Gesundhwes 2009;103(7):453–60
Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344(18):1343–50
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(6):393–403
Garber AJ, Duncan TG, Goodman AM, Mills DJ, Rohlf JL. Efficacy of metformin in type II diabetes: results of a double-blind, placebo-controlled, dose-response trial. Am J Med 1997;103(6):491–7
Hoffmann J, Spengler M. Efficacy of 24-week monotherapy with acarbose, metformin, or placebo in dietary-treated NIDDM patients: the Essen-II Study. Am J Med 1997;103(6):483–90
Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352(9131):854–65
Tessier D, Dawson K, Tetrault JP, Bravo G, Meneilly GS. Glibenclamide vs gliclazide in type 2 diabetes of the elderly. Diabet Med 1994;11(10):974–80
Arai K, Matoba K, Hirao K, et al. Present status of sulfonylurea treatment for type 2 diabetes in Japan: second report of a cross-sectional survey of 15,652 patients. Endocr J 2010;57(6):499–507
Aronoff S, Rosenblatt S, Braithwaite S, et al. Pioglitazone hydrochloride monotherapy improves glycemic control in the treatment of patients with type 2 diabetes: a 6-month randomized placebo-controlled dose-response study. The Pioglitazone 001 Study Group. Diabetes Care 2000;23(11):1605–11
Lebovitz HE, Dole JF, Patwardhan R, Rappaport EB, Freed MI. Rosiglitazone monotherapy is effective in patients with type 2 diabetes. J Clin Endocrinol Metab 2001;86(1):280–8
Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. Jama 1999;281(21):2005–12
Jones S, Benroubi M, Castell C, et al. Characteristics of patients with type 2 diabetes mellitus initiating insulin therapy: baseline data from the INSTIGATE study. Curr Med Res Opin 2009;25(3):691–700
Rathmann W, Haastert B, Roseman JM, Gries FA, Giani G. Prescription drug use and costs among diabetic patients in primary health care practices in Germany. Diabetes Care 1998;21(3):389–97
Rathmann W, Haastert B, Icks A, Giani G. Trends in outpatient prescription drug costs in diabetic patients in Germany, 1994–2004. Diabetes Care 2007;30(4):848–53
Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. Jama 1979;241(19):2035–8
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358(24):2545–59
Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358(24):2560–72
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360(2):129–39
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359(15):1577–89
29 Rakovac I, Plank J, Jeitler K, Beck P, Seereiner P, Mrak P, et al. Gesundheitsstatus der Typ-2-Diabetiker in Österreich aus der Sicht einer Qualitätssicherungs-Initiative. Wien Med Wochenschrift 2009;159(5–6):126–33
Flamm M, Winkler H, Panisch S, Kowatsch P, Klima G, Fürthauer G, et al. Quality of diabetes care in Austrian diabetic patients willing to participate in a DMP – at baseline. Wien Klin Wochenschrift 2011;123:436–43
Sönnichsen AC, Winkler H, Flamm M, Panisch S, Kowatsch P, Klima G, et al. The effectiveness oft he Austrian disease management programme for type 2 diabetes: a cluster-randomised controlled trial. BMC Family Practice 2010;11(1):86–95
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ludvik, B., Schernthaner, G. Diabetes Care Austria 2009: Register an allgemeinmedizinischen Ordinationen für PatientInnen mit Typ 2 Diabetes mellitus in Österreich. Wien Klin Wochenschr 124, 69–77 (2012). https://doi.org/10.1007/s00508-011-0120-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-011-0120-y