Abstract
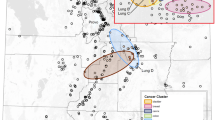
Our research group recently developed Q-statistics for evaluating space–time clustering in case–control studies with residential histories. This technique relies on time-dependent nearest-neighbor relationships to examine clustering at any moment in the life-course of the residential histories of cases relative to that of controls. In addition, in place of the widely used null hypothesis of spatial randomness, each individual’s probability of being a case is based instead on his/her risk factors and covariates. In this paper, we extend this approach to illustrate how alternative temporal orientations (e.g., years prior to diagnosis/recruitment, participant’s age, and calendar year) influence a spatial clustering pattern. These temporal orientations are valuable for shedding light on the duration of time between clustering and subsequent disease development (known as the empirical induction period), and for revealing age-specific susceptibility windows and calendar year-specific effects. An ongoing population-based bladder cancer case–control study is used to demonstrate this approach. Data collection is currently incomplete and therefore no inferences should be drawn; we analyze these data to demonstrate these novel methods. Maps of space–time clustering of bladder cancer cases are presented using different temporal orientations while accounting for covariates and known risk factors. This systematic approach for evaluating space–time clustering has the potential to generate novel hypotheses about environmental risk factors and provides insights into empirical induction periods, age-specific susceptibility, and calendar year-specific effects.




Similar content being viewed by others
References
Avruskin GA, Jacquez GM, Meliker JR, Slotnick MJ, Kaufmann AM, Nriagu JO (2004) Visualization and exploratory analysis of epidemiologic data using a novel space time information system. Int J Health Geogr 3:26
Besag J, Newell J (1991) The detection of clusters in rare diseases. J R Stat Soc A Stat 154:143–155
Cuzick J, Edwards R (1990) Spatial clustering for inhomogeneous populations. J R Stat Soc B Methodol 52:73–104
Goovaerts P, Jacquez GM (2004) Accounting for regional background and population size in the detection of spatial clusters and outliers using geostatistical filtering and spatial neutral models: the case of lung cancer in Long Island, New York. Int J Health Geogr 3:14
Hagerstrand T (1970) What about people in regional science? Pap Reg Sci Assoc 24:7–21
Hahn WC, Counter CM, Lundberg AS, Beijersbergen RL, Brooks MW, Weinberg RA (1999) Creation of human tumor cells with defined genetic elements. Nature 400:464–468
Han D, Rogerson PA, Nie J, Bonner MR, Vena JE, Vito D, Muti P, Trevisan M, Edge SB, Freudenheim JL (2004) Geographic clustering of residence in early life and subsequent risk of breast cancer (United States). Cancer Cause Control 15:921–929
Han D, Rogerson PA, Bonner MR, Nie J, Vena JE, Muti P, Trevisan M, Freudenheim JL (2005) Assessing spatio-temporal variability of risk surfaces using residential history data in a case control study of breast cancer. Int J Health Geogr 4:9
Hornsby K, Egenhofer M (2000) Identity-based change: a foundation for spatio-temporal knowledge representation. Int J Geogr Inf Sci 14:207–224
Jacquez GM (1996) Disease cluster statistics for imprecise space–time locations. Stat Med 15:873–885
Jacquez GM (2000) Spatial analysis in epidemiology: nascent science or a failure of GIS? J Geogr Syst 2:91–97
Jacquez GM (2004) Current practices in the spatial analysis of cancer: flies in the ointment. Int J Health Geogr 3:22
Jacquez GM, Kaufmann A, Meliker J, Goovaerts P, AvRuskin G, Nriagu J (2005) Global, local and focused geographic clustering for case–control data with residential histories. Environ Health 4:4
Jacquez GM, Meliker JR, AvRuskin GA, Goovaerts P, Kaufmann A, Wilson M, Nriagu J (2006) Case–control geographic clustering for residential histories accounting for risk factors and covariates. Int J Health Geogr 5:32
Jacquez GM, Meliker JR (2007) Case–control clustering for mobile populations. In: Fotheringham S, Rogerson P (eds) Handbook of spatial analysis. Sage Publications, Beverley Hills, CA (in press)
Kulldorff M, Nagarwalla N (1995) Spatial disease clusters: detection and inference. Stat Med 14:799–810
Kulldorff M, Huang L, Pickle L, Duczmal L (2006) An elliptic spatial scan statistic. Stat Med. doi:10.1002/sim.2490
Meliker JR, Slotnick MJ, AvRuskin GA, Kaufmann A, Jacquez GM, Nriagu JO (2005) Improving exposure assessment in environmental epidemiology: application of spatio-temporal visualization tools. J Geogr Syst 7:49–66
Ozonoff A, Webster T, Vieira V, Weinberg J, Ozonoff D, Aschengrau A (2005) Cluster detection methods applied to the Upper Cape Cod cancer data. Environ Health 4:19
Paulu C, Aschengrau A, Ozonoff D (2002) Exploring associations between residential location and breast cancer incidence in a case–control study. Environ Health Perspect 110:471–478
Rothman N (1981) Induction and latent periods. Am J Epidemiol 114:253–259
Sabel CE, Boyle PJ, Loytonen M, Gatrell AC, Jokelainen M, Flowerdew R, Maasilta P (2003) Spatial clustering of amyotrophic lateral sclerosis in Finland at place of birth and place of death. Am J Epidemiol 157:898–905
Silverman D, Morrison A, Devesa S (1996) Bladder cancer. In: Schottenfeld D, Fraumeni JF Jr (eds) Cancer epidemiology and prevention. Oxford University Press, New York, pp 1156–1179
Sinha G, Mark D (2005) Measuring similarity between geospatial lifelines in studies of environmental health. J Geogr Syst 7:115–136
Tango T, Takahashi K (2005) A flexibly shaped spatial scan statistic for detecting clusters. Int J Health Geogr 4:11
Turnbull BW, Iwano EJ, Burnett WS, Howe HL, Clark LC (1990) Monitoring for clusters of disease: application to leukemia incidence in upstate New York. Am J Epidemiol 132:S136–S143
Vieira V, Webster T, Weinberg J, Aschengrau A, Ozonoff D (2005) Spatial analysis of lung, colorectal, and breast cancer on Cape Cod: an application of generalized additive models to case–control data. Environ Health 4:11
Vogelestien B, Kinzler KW (1993) The multistep nature of cancer. Trends Genet 9:138–141
Waller LA, Turnbull BW (1993) The effects of scale on tests for disease clustering. Stat Med 12:1869–1884
Waller LA, Turnbull BW, Gustafsson G, Hjalmars U, Andersson B (1995) Detection and assessment of clusters of disease: an application to nuclear power plant facilities and childhood leukaemia in Sweden. Stat Med 14:3–16
Waller LA, Jacquez GM (1995) Disease models implicit in statistical tests of disease clustering. Epidemiology 6:584–590
Acknowledgments
We thank the participants for taking part in this study. We thank Dr. Jerome Nriagu of the University of Michigan for sharing the bladder cancer case–control dataset. Mr. Andy Kaufmann, Ms. Gillian Avruskin, and Dr. Pierre Goovaerts assisted with software development, database management, and construction of spatial null hypotheses. This research was funded by grants R43CA117171, R01CA096002, and R44CA092807 from the National Cancer Institute (NCI). Development of the STIS software was funded by grants R43 ES10220 from the National Institutes of Environmental Health Sciences (NIEHS) and R01 CA92669 from NCI. The views expressed in this publication are those of the researchers and do not necessarily represent those of NCI or NIEHS.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meliker, J.R., Jacquez, G.M. Space–time clustering of case–control data with residential histories: insights into empirical induction periods, age-specific susceptibility, and calendar year-specific effects. Stoch Environ Res Risk Assess 21, 625–634 (2007). https://doi.org/10.1007/s00477-007-0140-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00477-007-0140-3