Abstract
Background
Whether medical insurance impacts the timely diagnosis in chronic kidney disease (CKD) children is unknown. We aim to examine the extent to which insurance is associated with access to timely diagnosis and different stages of CKD among a large population of children in China.
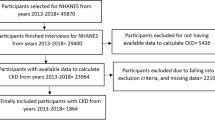
Methods
A retrospective, cross-sectional study based on China’s national hospitalized record database was carried out. Children aged 0–17 years diagnosed as CKD stages 1–5 between June 1, 2013, and December 31, 2018, were included. A diagnosis of advanced CKD stage (CKD stage 4 or 5) was the primary outcome. Multivariable logistic regression model adjusted for age, sex, cross-regional hospitalization, year of diagnosis, and cause of CKD was used to assess the association between insurance status and the stage of CKD when diagnosed.
Results
A total of 10,256 children (median [interquartile range, IQR] age, 12.4 [7.9, 15.4] years) were included. There were 4716 (46.0%) uninsured children in the included population. The insurance coverage was highest in children 13–17 years old (60.9%). The hospitalized charge was highest in stage 5 uninsured children (median [IQR], ¥13,000.89 [7640.63, 24,585.00]). More uninsured children are diagnosed in CKD stage 4 or 5 (48.1%) than insured children (47.5%). Uninsured children had higher odds (odds ratio [OR] 1.20, [95% CI, 1.08–1.32]) of receiving a diagnosis of CKD stage 4 or 5 compared with insured children.
Conclusions
Lack of medical insurance was associated with a more advanced stage of CKD when diagnosed in hospitalized children.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.



Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are not publicly available due to the Hospital Quality Monitoring System (HQMS) database management rules. Still, they are available from the corresponding author on reasonable request. The SAS codes used to produce the results in this article are available from the corresponding author on request.
References
Gandjour A, Armsen W, Wehmeyer W, Multmeier J, Tschulena U (2020) Costs of patients with chronic kidney disease in Germany. PLoS ONE 15:e0231375. https://doi.org/10.1371/journal.pone.0231375
Eknoyan G, Lameire N, Eckardt K, Kasiske B, Wheeler D, Levin A, Stevens P, Bilous R, Lamb E, Coresh J (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int 3:5–14
Levin A, Stevens PE (2011) Early detection of CKD: the benefits, limitations and effects on prognosis. Nat Rev Nephrol 7:446–457. https://doi.org/10.1038/nrneph.2011.86
Wouters OJ, O’Donoghue DJ, Ritchie J, Kanavos PG, Narva AS (2015) Early chronic kidney disease: diagnosis, management and models of care. Nat Rev Nephrol 11:491–502. https://doi.org/10.1038/nrneph.2015.85
Agrawal V, Jaar BG, Frisby XY, Chen S-C, Qiu Y, Li S, Whaley-Connell AT, McCullough PA, Bomback AS (2012) Access to health care among adults evaluated for CKD: findings from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 59:S5–S15. https://doi.org/10.1053/j.ajkd.2011.10.043
Morton RL, Schlackow I, Mihaylova B, Staplin ND, Gray A, Cass A (2016) The impact of social disadvantage in moderate-to-severe chronic kidney disease: an equity-focused systematic review. Nephrol Dial Transplant 31:46–56. https://doi.org/10.1093/ndt/gfu394
Hall YN, Rodriguez RA, Boyko EJ, Chertow GM, O’Hare AM (2009) Characteristics of uninsured Americans with chronic kidney disease. J Gen Intern Med 24:917–922. https://doi.org/10.1007/s11606-009-1028-3
Kutner NG, Zhang R, Huang Y, Herzog CA (2006) Cardiac rehabilitation and survival of dialysis patients after coronary bypass. J Am Soc Nephrol 17:1175–1180. https://doi.org/10.1681/ASN.2005101027
Kausz AT, Obrador GT, Arora P, Ruthazer R, Levey AS, Pereira BJG (2000) Late initiation of dialysis among women and ethnic minorities in the United States. J Am Soc Nephrol 11:2351–2357. https://doi.org/10.1681/asn.V11122351
Calderon-Margalit R, Golan E, Twig G, Leiba A, Tzur D, Afek A, Skorecki K, Vivante A (2018) History of childhood kidney disease and risk of adult end-stage renal disease. N Engl J Med 378:428–438. https://doi.org/10.1056/NEJMoa1700993
Holl JL, Szilagyi PG, Rodewald LE, Shone LP, Zwanziger J, Mukamel DB, Trafton S, Dick AW, Barth R, Raubertas RF (2000) Evaluation of New York State’s Child Health Plus: access, utilization, quality of health care, and health status. Pediatrics 105:711–718
Lei X, Lin W (2009) The New Cooperative Medical Scheme in rural China: does more coverage mean more service and better health? Health Econ 18(Suppl 2):S25-46. https://doi.org/10.1002/hec.1501
Slifkin RT, Freeman VA, Silberman P (2002) Effect of the North Carolina State Children’s Health Insurance Program on beneficiary access to care. Arch Pediatr Adolesc Med 156:1223–1229. https://doi.org/10.1001/archpedi.156.12.1223
Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, McInerny T (2004) Improved access and quality of care after enrollment in the New York State Children’s Health Insurance Program (SCHIP). Pediatrics 113:e395-404. https://doi.org/10.1542/peds.113.5.e395
Mou S, Zhou Z (2017) Health performance evaluation of the New Rural Cooperative Medical Insurance and the Basic Medical Insurance for urban residents on children. Social Security Studies pp.45–54
Liu W, Meng Z, Han X (2016) The impact of medical insurance on children’s health. Insurance studies 25:77–87. https://doi.org/10.13497/j.-cnki.is.2016.04.008
Shi X, Shi Y, Zhang L, Gan L, Zhong X, Huang Y, Yao C, Wang Y, Dong C, Liu B, Wang F, Wang H, Ding J (2021) Analysis of chronic kidney disease among national hospitalization data with 14 million children. BMC Nephrol 22:195. https://doi.org/10.1186/s12882-021-02383-1
Interaction effect in multiple regression: essentials-articles-STHDA [Internet]. [cited 2021 Dec 10]. Available from: http://www.sthda.com/english/articles/40-regression-analysis/164-interaction-effect-in-multiple-regression-essentials/
Brand JPL (1999) Development, implementation and evaluation of multiple imputation strategies for the statistical analysis of incomplete data sets.
van Buuren S (2007) Multiple imputation of discrete and continuous data by fully conditional specification. Stat Methods Med Res 16:219–242. https://doi.org/10.1177/0962280206074463
Levey AS, Coresh J (2012) Chronic kidney disease. Lancet 379:165–180. https://doi.org/10.1016/s0140-6736(11)60178-5
He G, Li C, Zhong X, Wang F, Wang H, Shi Y, Gan L, Ding J (2021) Risk factors for progression of chronic kidney disease with glomerular etiology in hospitalized children. Front Pediatr 9:752717. https://doi.org/10.3389/fped.2021.752717
Babayev R, Whaley-Connell A, Kshirsagar A, Klemmer P, Navaneethan S, Chen SC, Li S, McCullough PA, Bakris G, Bomback A, KEEP Investigators (2013) Association of race and body mass index with ESRD and mortality in CKD stages 3–4: results from the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 61:404–412. https://doi.org/10.1053/j.ajkd.2012.11.038
Halpern MT, Ward EM, Pavluck AL, Schrag NM, Bian J, Chen AY (2008) Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol 9:222–231. https://doi.org/10.1016/s1470-2045(08)70032-9
Yuan B, Li J, Wu L, Wang Z (2019) Multi-level social health insurance system in the age of frequent employment change: the urban unemployment-induced insurance transition and healthcare utilization in China. Healthcare (Basel) 7:77. https://doi.org/10.3390/healthcare7020077
Wang H (2009) A dilemma of Chinese healthcare reform: how to re-define government roles? China Econ Rev 20:598–604
China to improve medical insurance system to better meet people’s healthcare needs—Xinhua [Internet]. [cited 2022 Jan 2]. Available from: http://www.news.cn/english/2021-09/15/c_1310189941.htm
Yip WC, Hsiao WC, Chen W, Hu S, Ma J, Maynard A (2012) Early appraisal of China’s huge and complex health-care reforms. Lancet 379:833–842. https://doi.org/10.1016/s0140-6736(11)61880-1
Chen YY, Xu XH, Liu GM, Xiang GP (2016) Brief introduction of medical insurance system in China. Asia Pac J Oncol Nurs 3:51–53
National Bureau of Statistics of China 2019 China statistical yearbook China Statistics Press Beijing
Wang C (2020) The effective coverage rate and distribution characteristics of China’s Basic Medical Insurance: analysis based on multi-source data. Chinese Social Security Review 4:67–84
Meng Q, Fang H, Liu X, Yuan B, Xu J (2015) Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet 386:1484–1492. https://doi.org/10.1016/S0140-6736(15)00342-6
Li L, Zhou Q, Yin T, Ji Z, Zhang L (2021) Does the direct settlement policy of trans-provincial outpatient expenses aggravate the siphoning effect? An empirical study on Yangtze River Delta, China. Int J Environ Res Public Health 18:10001. https://doi.org/10.3390/ijerph181910001
Zhang L-F, Chen Y-G (2013) Analysis of the factors affecting the children participating in the medical insurance: taking the Shanghai children’s hospitalization assistance fund as an example. Statistics & Information Forum, p 06.
Jiao-yuan L, Xiang-ming F (2018) An analysis and reflection on the participation and reimbursement of children’s social medical insurance in China: based on the data of China family panel studies. Journal of Jiangxi University of Finance and Economics:02
Full text: report on China’s central and local budgets (2019) [Internet]. [cited 2022 Jan 5]. Available from: http://en.npc.gov.cn.cdurl.cn/2019-03/18/c_674744.htm
Ridic G, Gleason S, Ridic O (2012) Comparisons of health care systems in the United States, Germany and Canada. Mater Sociomed 24:112–120. https://doi.org/10.5455/msm.2012.24.112-120
Dou G, Wang Q, Ying X (2018) Reducing the medical economic burden of health insurance in China: achievements and challenges. Biosci Trends 12:215–219. https://doi.org/10.5582/bst.2018.01054
Cao Q, Shi L, Wang H, Dong K (2012) Report from China: health insurance in China—evolution, current status, and challenges. Int J Health Serv 42:177–195. https://doi.org/10.2190/HS.42.2.b
Tang S, Tao J, Bekedam H (2012) Controlling cost escalation of healthcare: making universal health coverage sustainable in China. BMC Public Health 12:S8. https://doi.org/10.1186/1471-2458-12-S1-S8
National Health and Family Planning Commission of China (2016) Statistical yearbook of health and family planning in China 2016. Union Medical University Press.
National Development and Reform Commission (2015) Guidance on efforts to provide catastrophic disease insurance to urban and rural residents
Acknowledgements
The authors thank the Bureau of Medical Administration and Medical Service Supervision, NHC of the People’s Republic of China, all study participants, and the original data creators for forming the dataset. We thank Yangfeng Wu, M.D., Ph.D., Peking University Clinical Research Institute, for his helpful advice in revising the manuscript. We thank Ying Shi, B.M.S., and Lanxia Gan, B.S., China Standard Medical Information Research Center, Shenzhen, China, for their helpful advice in the analysis process.
Author information
Authors and Affiliations
Contributions
G.H. contributed to the design, analysis of the data, and drafting of the article; C.L. performed the statistical analysis and drafting the article; S.W. contributed to the design and interpretation of the data; H.W. and J.D. are responsible for supervision for design, interpretation of the data, and revising the article. Each author contributed important intellectual content during this article drafting and revision and approved the final version of the article.
Corresponding authors
Ethics declarations
Ethics approval
This retrospective study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was reviewed and approved by the Ethics Committee Board of Peking University First Hospital (approval number: 2021 [009]).
Consent to participate
This research study was conducted retrospectively from data obtained for clinical and quality monitoring purposes. The use of this de-identified dataset in this study was approved by the Ethics Committee Board of Peking University First Hospital with a waiver of informed consent.
Consent for publication
This retrospective study used a de-identified dataset. Consent to publish from participants could not be applied in this study.
Conflict of interest
The authors declare no competing interests.
Research resource identifiers (RRID)
Software: SAS software 9.4 (SAS Inc., Cary, NC, USA), RRID: SCR_008567.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, G., Li, C., Wang, S. et al. Association of insurance status with chronic kidney disease stage at diagnosis in children. Pediatr Nephrol 37, 2705–2714 (2022). https://doi.org/10.1007/s00467-022-05493-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05493-6