Abstract
Background
Emerging data suggest evidence of organ hypoperfusion during continuous kidney replacement therapy (CKRT). To facilitate kidney and global recovery, we must understand the hemodynamic risks associated with CKRT. We aimed to investigate frequency of hemodynamic instability and association with patient outcomes in pediatric CKRT.
Methods
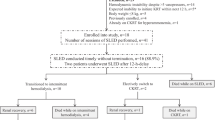
In a single-center study of CKRT patients between September 2016 and October 2018, we collected hemodynamic data using archived high-resolution physiologic data before and after connection. Primary outcome was hypotension defined as ≥ 20% decrease in baseline mean arterial pressure (MAP) for ≥ 2 consecutive minutes in the 60 min following connection. Secondary outcomes were tachycardia (≥ 20% increase in heart rate (HR)) and hemodynamic interventions.
Results
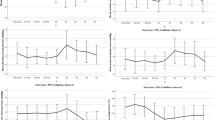
Seventy-one patients median age 54 months (IQR 7–144), weight 16.7 kg (IQR 8–41), on hemodiafiltration had 304 filter connections, 4 (IQR 1–7) filters per patient; the median duration of CKRT was 9 days (IQR 3–20). The most common CKRT indication was AKI with fluid overload (48/71, 69%). There were 78 (27%) hypotension and 42 (14%) tachycardia events; cumulative duration of hypotension was 14 min IQR (3–31.75). Teams provided intervention in 17/304 (6%) of connections. Pediatric Logistic Organ Dysfunction 2 was the only independent predictor of hypotension (aOR 2.12 (CI 1.02–4.41)).
Conclusions
One in four and one in six pediatric CKRT filter connections were complicated by hypotension and tachycardia, respectively. Higher illness severity at CKRT initiation was independently associated with hypotension. Impact of CKRT-associated hemodynamic instability on global patient outcomes requires further targeted study.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information



Similar content being viewed by others
References
Macedo E, Cerdá J, Hingorani S, Hou J et al (2018) Recognition and management of acute kidney injury in children: the ISN 0by25 Global Snapshot study. PLoS ONE 13:e0196586. https://doi.org/10.1371/journal.pone.0196586
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators AWARE (2017) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/NEJMoa1611391
Annigeri RA, Ostermann M, Tolwani A, Vazquez-Rangel A et al (2017) Renal support for acute kidney injury in the developing world. Kidney Int Rep 2:559–578. https://doi.org/10.1016/j.ekir.2017.04.006
(2011) Section 5: dialysis interventions for treatment of AKI. Kidney Int Suppl 2:89–115. https://doi.org/10.1038/kisup.2011.35
Robinson CH, Jeyakumar N, Luo B, Wald R et al (2021) Long-term kidney outcomes following dialysis-treated childhood acute kidney injury: a population-based cohort study. J Am Soc Nephrol 32:2005–2019. https://doi.org/10.1681/ASN.2020111665
Zappitelli M, Parikh CR, Kaufman JS, Go AS, Kimmel PL, Hsu CY, Coca SG, Chinchilli VM, Greenberg JH, Moxey-Mims MM, Ikizler TA, Cockovski V, Dyer AM, Devarajan P, ASsessment Serial Evaluation and Subsequent Sequelae in Acute Kidney Injury (ASSESS-AKI) Investigators, (2020) Acute kidney injury and risk of CKD and hypertension after pediatric cardiac surgery. Clin J Am Soc Nephrol 15:1403–1412. https://doi.org/10.2215/CJN.00150120
Douvris A, Zeid K, Hiremath S, Bagshaw SM et al (2019) Mechanisms for hemodynamic instability related to renal replacement therapy: a narrative review. Intensive Care Med 45:1333–1346. https://doi.org/10.1007/s00134-019-05707-w
Slessarev M, Salerno F, Ball IM, McIntyre CW (2019) Continuous renal replacement therapy is associated with acute cardiac stunning in critically ill patients. Hemodial Int 23:325–332. https://doi.org/10.1111/hdi.12760
Brophy PD, Mottes TA, Kudelka TL, McBryde KD et al (2001) AN-69 membrane reactions are pH-dependent and preventable. Am J Kidney Dis 38:173–178. https://doi.org/10.1053/ajkd.2001.25212
Santiago MJ, López-Herce J, Urbano J, Solana MJ et al (2009) Complications of continuous renal replacement therapy in critically ill children: a prospective observational evaluation study. Crit Care 13:R184. https://doi.org/10.1186/cc8172
Fernández S, Santiago MJ, González R, Urbano J et al (2019) Hemodynamic impact of the connection to continuous renal replacement therapy in critically ill children. Pediatr Nephrol 34:163–168. https://doi.org/10.1007/s00467-018-4047-7
Fernández Lafever SN, López J, González R, Solana MJ et al (2021) Hemodynamic disturbances and oliguria during continuous kidney replacement therapy in critically ill children. Pediatr Nephrol 36:1889–1899. https://doi.org/10.1007/s00467-020-04804-z
Riley AA, Watson M, Smith C, Guffey D et al (2018) Pediatric continuous renal replacement therapy: have practice changes changed outcomes? A large single-center ten-year retrospective evaluation. BMC Nephrol 19:268. https://doi.org/10.1186/s12882-018-1068-1
Haque IU, Zaritsky AL (2007) Analysis of the evidence for the lower limit of systolic and mean arterial pressure in children. Pediatr Crit Care Med 8:138–144. https://doi.org/10.1097/01.PCC.0000257039.32593.DC
McIntosh AM, Tong S, Deakyne SJ, Davidson JA, Scott HF (2017) Validation of the vasoactive-inotropic score in pediatric sepsis. Pediatr Crit Care Med 18:750–757. https://doi.org/10.1097/PCC.0000000000001191
Leteurtre S, Duhamel A, Salleron J, Grandbastien B et al (2013) PELOD-2: an update of the PEdiatric Logistic Organ Dysfunction score. Crit Care Med 41:1761–1773. https://doi.org/10.1097/CCM.0b013e31828a2bbd
Leteurtre S, Duhamel A, Deken V, Lacroix J, Leclerc F; Groupe Francophone de Réanimation et Urgences Pédiatriques (2015) Daily estimation of the severity of organ dysfunctions in critically ill children by using the PELOD-2 score. Crit Care 19:324. https://doi.org/10.1186/s13054-015-1054-y
Billings FT IV, Shaw AD (2014) Clinical Trial endpoints in acute kidney injury. Nephron Clin Pract 127:89–93. https://doi.org/10.1159/000363725
Schwartz GJ, Haycock GB, Edelmann CM, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
Eytan D, Goodwin AJ, Greer R, Guerguerian A-M, Laussen PC (2017) Heart rate, and blood pressure centile curves and distributions by age of hospitalized critically ill children. Front Pediatr 5:52. https://doi.org/10.3389/fped.2017.00052
Roberts JS, Yanay O, Barry D (2020) Age-based percentiles of measured mean arterial pressure in pediatric patients in a hospital setting. Pediatr Crit Care Med 21:e759–e768. https://doi.org/10.1097/PCC.0000000000002495
Weiss SL, Peters MJ, Alhazzani W, Agus MSD et al (2020) Surviving Sepsis Campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatr Crit Care Med 21:e52–e106. https://doi.org/10.1097/PCC.0000000000002198
Panwar R, Tarvade S, Lanyon N, Saxena M et al (2020) Relative hypotension and adverse kidney-related outcomes among critically ill patients with shock. A Multicenter, Prospective Cohort Study. Am J Respir Crit Care Med 202:1407–1418. https://doi.org/10.1164/rccm.201912-2316OC
Wong BT, Chan MJ, Glassford NJ, Mårtensson J, Bion V, Chai SY, Oughton C, Tsuji IY, Candal CL, Bellomo R (2015) Mean arterial pressure and mean perfusion pressure deficit in septic acute kidney injury. J Crit Care 30:975–981. https://doi.org/10.1016/j.jcrc.2015.05.003
Faraway JJ (2006) Extending the linear model with R: generalized linear, mixed effects and nonparametric regression models. Chapman & Hall/CRC, Boca Raton, FL
Harty J (2014) Prevention and management of acute kidney injury. Ulster Med J 83:149–157
Hatherill M, Tibby SM, Hilliard T, Turner C, Murdoch IA (1999) Adrenal insufficiency in septic shock. Arch Dis Child 80:51–55. https://doi.org/10.1136/adc.80.1.51
Badke CM, Marsillio LE, Weese-Mayer DE, Sanchez-Pinto LN (2018) Autonomic nervous system dysfunction in pediatric sepsis. Front Pediatr 6:280. https://doi.org/10.3389/fped.2018.00280
Erickson SL, Killien EY, Wainwright M, Mills B, Vavilala MS (2021) Mean arterial pressure and discharge outcomes in severe pediatric traumatic brain injury. Neurocrit Care 34:1017–1025. https://doi.org/10.1007/s12028-020-01121-z
Panchal AR, Bartos JA, Cabañas JG, Donnino MW et al (2020) Part 3: adult basic and advanced life support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142:S366–S468. https://doi.org/10.1161/CIR.0000000000000916
Luce WA, Hoffman TM, Bauer J (2007) Bench-to-bedside review: developmental influences on the mechanisms, treatment and outcomes of cardiovascular dysfunction in neonatal versus adult sepsis. Crit Care 11:228. https://doi.org/10.1186/cc6091
Naorungroj T, Neto AS, Zwakman-Hessels L, Fumitaka Y et al (2020) Mediators of the impact of hourly net ultrafiltration rate on mortality in critically ill patients receiving continuous renal replacement therapy. Crit Care Med 48:e934–e942. https://doi.org/10.1097/CCM.0000000000004508
Phillips GJ, Davies JG, Olliff CJ, Kingswood C, Street M (1998) Use of in vitro models of haemofiltration and haemodiafiltration to estimate dosage regimens for critically ill patients prescribed cefpirome. J Clin Pharm Ther 23:353–359. https://doi.org/10.1046/j.1365-2710.1998.00169.x
Murugan R, Kerti SJ, Chang C-CH, Gallagher M et al (2019) Association of net ultrafiltration rate with mortality among critically ill adults with acute kidney injury receiving continuous venovenous hemodiafiltration: a secondary analysis of the randomized evaluation of normal vs augmented level (RENAL) of renal replacement therapy Trial. JAMA Netw Open 2:e195418. https://doi.org/10.1001/jamanetworkopen.2019.5418
Acknowledgements
The authors gratefully acknowledge the support of Doctor Jorge A. CossBu, MD.
Funding
Internal funding from the Baylor College of Medicine supported this study. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Thadani, S., Fogarty, T., Mottes, T. et al. Hemodynamic instability during connection to continuous kidney replacement therapy in critically ill pediatric patients. Pediatr Nephrol 37, 2167–2177 (2022). https://doi.org/10.1007/s00467-022-05424-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05424-5