Abstract
Background
Cardiac surgery-associated acute kidney injury (AKI) is associated with increased morbidity and mortality in both adults and children.
Objectives
This study aimed to identify clinical risk factors for AKI following cardiac surgery in the pediatric population.
Data sources
PubMed/MEDLINE, Embase, Scopus, and reference lists of relevant articles were searched for studies published by August 2020.
Study eligibility criteria
Studies were included if (1) the population consisted of pediatric patients (< 18 years old), (2) patients underwent cardiac surgery, (3) risk factors were compared between patients who developed AKI and those who did not, and (4) studies were prospective or retrospective observational studies or randomized controlled trials.
Participants and interventions
Children undergoing pediatric cardiac surgery.
Study appraisal and synthesis methods
Random-effects meta-analysis was performed, comparing potential risk factors between pediatric patients who developed CS-AKI and those who did not.
Results
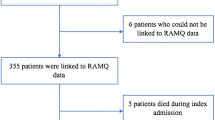
Sixty-one publications including a total of 19,680 participants (AKI: 7257 participants; no AKI: 12,423 participants) were included from studies published between 2008 and 2020. The pooled estimated incidence of AKI was 34.3% (95% confidence interval 30.0–38.8%, I2 = 96.8%). Binary risk factors that were significantly and consistently associated with AKI were the presence of pulmonary hypertension, cyanotic heart disease, univentricular heart, risk adjustment for congenital heart surgery 1 (RACHS-1) score ≥ 3, vasopressor use, cardiopulmonary bypass use, reoperation, and sepsis. Significant continuous risk factors included younger age, lower body weight, lower preoperative creatinine, higher preoperative estimated glomerular filtration rate (eGFR), higher RACHS-1 score, longer surgery time, longer cardiopulmonary bypass time, longer aortic cross-clamp time, and higher red blood cell transfusion volume.
Limitations
Results are limited by heterogeneity and potential residual confounding.
Conclusions and implications of key findings
Our meta-analysis identified clinical risk factors that are associated with AKI in children undergoing cardiac surgery. This might help clinicians anticipate and manage more carefully this population and implement standardized preventive strategies.
Systematic review registration number
CRD42021262699.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
The code used for this study will be made available from the corresponding author, upon reasonable request.
Abbreviations
- AKI:
-
Acute kidney injury
- AKIN:
-
Acute kidney injury network
- CI:
-
Confidence interval
- CPB:
-
Cardiopulmonary bypass
- eCrCl:
-
Estimated creatinine clearance
- eGFR:
-
Estimated glomerular filtration rate
- KDIGO:
-
Kidney disease improving global outcomes
- MD:
-
Mean difference
- MOOSE:
-
Meta-analysis of observational studies in epidemiology
- OR:
-
Odds ratio
- PRISMA:
-
Preferred reporting items for systematic reviews meta-analyses
- PROSPERO:
-
International prospective register of systematic reviews
- RACHS-1:
-
Risk adjustment for congenital heart surgery 1
- RIFLE:
-
Risk for renal dysfunction, Injury to the kidney, failure of kidney function, loss of kidney function and end-stage renal disease
- SCr:
-
Serum creatinine
References
Hoste EAJ, Kellum JA, Selby NM, Zarbock A, Palevsky PM, Bagshaw SM, Goldstein SL, Cerdá J, Chawla LS (2018) Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol 14:607–625
Van den Eynde J, Rotbi H, Gewillig M, Kutty S, Allegaert K (2021) In-Hospital outcomes of acute kidney injury after pediatric cardiac surgery : a meta-analysis. Front Pediatr 9:733744. https://doi.org/10.3389/fped.2021.733744
Page MJ, McKenzie JE, Bossuyt PM, Boutron I et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5:13. https://doi.org/10.1186/1471-2288-5-13
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Br Med J 327:557–560
DerSimonian R, Kacker R (2007) Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 28:105–114. https://doi.org/10.1016/j.cct.2006.04.004
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088. https://doi.org/10.2307/2533446
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Br Med J 315:629–634. https://doi.org/10.1136/bmj.316.7129.469
Blinder JJ, Asaro LA, Wypij D, Selewski DT, Agus MSD, Gaies M, Ferguson MA (2017) Acute kidney injury after pediatric cardiac surgery: a secondary analysis of the safe pediatric euglycemia after cardiac surgery trial. Pediatr Crit Care Med 18:638–646. https://doi.org/10.1097/PCC.0000000000001185
Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL (2007) Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int 71:1028–1035. https://doi.org/10.1038/sj.ki.5002231
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron 120:c179–c184. https://doi.org/10.1159/000339789
Mehta RL, Kellum JA, Shah SV, Molitoris BA et al (2007) Acute kidney injury network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 11:R31. https://doi.org/10.1186/cc5713
Selewski DT, Charlton JR, Jetton JG, Guillet R, Mhanna MJ, Askenazi DJ, Kent AL (2015) Neonatal acute kidney injury. Pediatrics 136:e463–e473. https://doi.org/10.1542/peds.2014-3819
Mooney JF, Ranasinghe I, Chow CK, Perkovic V, Barzi F, Zoungas S, Holzmann MJ, Welten GM, Biancari F, Wu VC, Tan TC, Cass A, Hillis GS (2013) Preoperative estimates of glomerular filtration rate as predictors of outcome after surgery: a systematic review and meta-analysis. Anesthesiology 118:809–824
Brenner BM, Lawler EV, Mackenzie HS (1996) The hyperfiltration theory: a paradigm shift in nephrology. Kidney Int 49:1774–1777
Algaze CA, Koth AM, Faberowski LW, Hanley FL, Krawczeski CD, Axelrod DM (2017) Acute kidney injury in patients undergoing the extracardiac Fontan operation with and without the use of cardiopulmonary bypass. Pediatr Crit Care Med 18:34–43. https://doi.org/10.1097/PCC.0000000000000984
Bojan M, Lopez-Lopez V, Pouard P, Falissard B, Journois D (2013) Limitations of early serum creatinine variations for the assessment of kidney injury in neonates and infants with cardiac surgery. PLoS One 8:e79308. https://doi.org/10.1371/JOURNAL.PONE.0079308
Springate JE, Christensen SL, Feld LG (1992) Serum creatinine level and renal function in children. Am J Dis Child 146:1232–1235. https://doi.org/10.1001/archpedi.1992.02160220118036
Boer DP, De Rijke YB, Hop WC, Cransberg K, Dorresteijn EM (2010) Reference values for serum creatinine in children younger than 1 year of age. Pediatr Nephrol 25:2107–2113. https://doi.org/10.1007/s00467-010-1533-y
MdRalib A, Pickering JW, Shaw GM, Endre ZH (2013) The urine output definition of acute kidney injury is too liberal. Crit Care 173:1–11. https://doi.org/10.1186/CC12784
Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL (2016) Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med 376:11–20. https://doi.org/10.1056/NEJMOA1611391
Jetton JG, Boohaker LJ, Sethi SK, Wazir S et al (2017) Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Heal 1:184–194. https://doi.org/10.1016/S2352-4642(17)30069-X
Fuhrman DY (2021) The role of renal functional reserve in predicting acute kidney injury. Crit Care Clin 37:399–407. https://doi.org/10.1016/J.CCC.2020.11.008
Kalligeros M, Karageorgos SA, Shehadeh F, Zacharioudakis IM, Mylonakis E (2019) The association of acute kidney injury with the concomitant use of vancomycin and piperacillin-tazobactam in children: a systematic review and meta-analysis. Antimicrob Agents Chemother 63:e01572–01519. https://doi.org/10.1128/AAC.01572-19
Paparella D, Yau TM, Young E (2002) Cardiopulmonary bypass induced inflammation: pathophysiology and treatment. An update. Eur J Cardiothorac Surg 21:232–244
Eaton MP, Iannoli EM (2011) Coagulation considerations for infants and children undergoing cardiopulmonary bypass. Pediatr Anesth 21:31–42. https://doi.org/10.1111/j.1460-9592.2010.03467.x
Piggott KD, Soni M, Decampli WM, Ramirez JA, Holbein D, Fakioglu H, Blanco CJ, Pourmoghadam KK (2015) Acute kidney injury and fluid overload in neonates following surgery for congenital heart disease. World J Pediatr Congenit Heart Surg 6:401–406. https://doi.org/10.1177/2150135115586814
Morgan CJ, Zappitelli M, Robertson CMT, Alton GY, Sauve RS, Joffe AR, Ross DB, Rebeyka IM (2013) Risk factors for and outcomes of acute kidney injury in neonates undergoing complex cardiac surgery. J Pediatr 162:120-127.e1. https://doi.org/10.1016/j.jpeds.2012.06.054
Boehne M, Sasse M, Karch A, Dziuba F, Horke A, Kaussen T, Mikolajczyk R, Beerbaum P, Jack T (2017) Systemic inflammatory response syndrome after pediatric congenital heart surgery: Incidence, risk factors, and clinical outcome. J Card Surg 32:116–125. https://doi.org/10.1111/jocs.12879
Rosner MH, Okusa MD (2006) Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol 1:19–32. https://doi.org/10.2215/CJN.00240605
Wheeler DS, Jeffries HE, Zimmerman JJ, Wong HR, Carcillo JA (2011) Sepsis in the pediatric cardiac intensive care unit. World J Pediatr Congenit Heart Surg 2:393. https://doi.org/10.1177/2150135111403781
Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM et al (2016) Acute kidney injury in pediatric severe sepsis: an independent risk factor for death and new disability. Crit Care Med 44:2241–2250. https://doi.org/10.1097/CCM.0000000000002007
Zarjou A, Agarwal A (2011) Sepsis and acute kidney injury. J Am Soc Nephrol 22:999–1006. https://doi.org/10.1681/ASN.2010050484
Li D, Niu Z, Huang Q, Sheng W, Wang T (2020) A meta-analysis of the incidence rate of postoperative acute kidney injury in patients with congenital heart disease. BMC Nephrol 21:350. https://doi.org/10.1186/s12882-020-02005-2
Dittrich S, Haas N, Bührer C, Müller C, Dähnert I, Lange P (2007) Renal impairment in patients with long-standing cyanotic congenital heart disease. Acta Paediatr 87:949–954. https://doi.org/10.1111/j.1651-2227.1998.tb01764.x
Lee D, Levin A, Kiess M, Sexsmith G, Chakrabarti S, Barlow A, Human D, Grewal J (2018) Chronic kidney damage in the adult Fontan population. Int J Cardiol 257:62–66. https://doi.org/10.1016/j.ijcard.2017.11.118
Abman SH, Hansmann G, Archer SL, Ivy DD et al (2015) Pediatric pulmonary hypertension. Circulation 132:2037–2099
Ronco C, McCullough P, Anker SD, Anand I et al (2010) Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. Eur Heart J 31:703–711. https://doi.org/10.1093/EURHEARTJ/EHP507
Naranjo M, Lo KB, Mezue K, Rangaswami J (2019) Effects of pulmonary hypertension and right ventricular function in short and long-term kidney function. Curr Cardiol Rev 15:3. https://doi.org/10.2174/1573403X14666181008154215
Kozlik-Feldmann R, Hansmann G, Bonnet D, Schranz D, Apitz C, Michel-Behnke I (2016) Pulmonary hypertension in children with congenital heart disease (PAH-CHD, PPHVD-CHD). Expert consensus statement on the diagnosis and treatment of paediatric pulmonary hypertension. The European paediatric pulmonary vascular disease network, endorsed by ISHLT and DGPK. Heart 102:42–48. https://doi.org/10.1136/heartjnl-2015-308378
Ostermann M, Liu K (2017) Pathophysiology of AKI. Best Pract Res Clin Anaesthesiol 31:305–314
Mårtensson J, Martling CR, Bell M (2012) Novel biomarkers of acute kidney injury and failure: clinical applicability. Br J Anaesth 109:843–850
Coca SG, Yalavarthy R, Concato J, Parikh CR (2008) Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int 73:1008–1016
Bellos I, Iliopoulos DC, Perrea DN (2019) Pharmacological interventions for the prevention of acute kidney injury after pediatric cardiac surgery: a network meta-analysis. Clin Exp Nephrol 23:782–791. https://doi.org/10.1007/s10157-019-01706-9
Cooper DS, Claes D, Goldstein SL, Bennett MR, Ma Q, Devarajan P, Krawczeski CD (2016) Follow-up renal assessment of injury long-term after acute kidney injury (FRAIL-AKI). Clin J Am Soc Nephrol 11:21–29. https://doi.org/10.2215/CJN.04240415
Morgan C, Al-Aklabi M, Garcia Guerra G (2015) Chronic kidney disease in congenital heart disease patients: a narrative review of evidence. Can J Kidney Heal Dis 2:27. https://doi.org/10.1186/s40697-015-0063-8
Acknowledgements
J. Van den Eynde was supported by the Belgian American Educational Foundation.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JVDE: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Visualization; Writing—original draft; Writing—review & editing. BD: Conceptualization; Data curation; Investigation; Writing—original draft; Writing—review & editing. XJ: Conceptualization; Data curation; Investigation; Writing—original draft; Writing—review & editing. IP: Conceptualization; Data curation; Investigation; Writing—original draft; Writing—review & editing. HR: Conceptualization; Data curation; Investigation; Writing—original draft; Writing—review & editing. MG: Conceptualization; Investigation; Supervision; Writing—review & editing. SK: Conceptualization; Investigation; Supervision; Writing—review & editing. DM: Conceptualization; Investigation; Supervision; Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
M. Gewillig is proctor for Edwards and Medtronic. S. Kutty is consultant for GE Healthcare. All other authors declare that they have no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Van den Eynde, J., Delpire, B., Jacquemyn, X. et al. Risk factors for acute kidney injury after pediatric cardiac surgery: a meta-analysis. Pediatr Nephrol 37, 509–519 (2022). https://doi.org/10.1007/s00467-021-05297-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-021-05297-0