Abstract
Background
Existing risk adjustment models for solid organ transplantation omit socioeconomic status (SES). With limited data available on transplant candidates’ SES, linkage of transplant outcomes data to geographic SES measures has been proposed. We investigate the utility of county SES for understanding differences in pediatric kidney transplantation (KTx) outcomes.
Methods
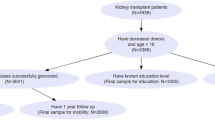
We identified patients < 18 years of age receiving first-time KTx using United Network for Organ Sharing registry data in two eras: 2006–2010 and 2011–2015, corresponding to periods of county SES data collection. In each era, counties were ranked by 1-year rates of survival with intact graft, and by county SES score. We used Spearman correlation (ρ) to evaluate the association between county rankings on SES and transplant outcomes in each era and consistency between these measures across eras. We also evaluated the utility of county SES for improving prediction of individual KTx outcomes.
Results
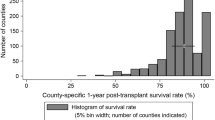
The analysis included 2972 children and 108 counties. County SES and transplant outcomes were not correlated in either 2006–2010 (ρ = 0.06; p = 0.525) or 2011–2015 (ρ = 0.162, p = 0.093). County SES rankings were strongly correlated between eras (ρ = 0.99, p < 0.001), whereas county rankings of transplant outcomes were not correlated between eras (ρ = 0.16, p = 0.097). Including county SES quintile in individual-level models of transplant outcomes did not improve model predictive utility.
Conclusions
Pediatric kidney transplant outcomes are unstable from period to period at the county level and are not correlated with county-level SES. Appropriate adjustment for SES disparities in transplant outcomes could require further collection of detailed individual SES data.

Similar content being viewed by others
References
Hart A, Smith JM, Skeans MA, Gustafson SK, Stewart DE, Cherikh WS, Wainright JL, Kucheryavaya A, Woodbury M, Snyder JJ, Kasiske BL, Israni AK (2017) OPTN/SRTR 2015 annual data report: kidney. Am J Transplant 17(Suppl 1):21–116
Valapour M, Skeans MA, Smith JM, Edwards LB, Cherikh WS, Uccelini K, Israni AK, Snyder JJ, Kasiske BL (2017) OPTN/SRTR 2015 annual data report: lung. Am J Transplant 17(Suppl 1):357–424
Frequently asked questions about multiple listing and waiting time transfer (2017) United Network for Organ Sharing. Available at: https://www.unos.org/wp-content/uploads/unos/Multiple_Listing.pdf. Accessed January 15, 2018
Howard RJ, Cornell DL, Schold JD (2009) CMS oversight, OPOs and transplant centers and the law of unintended consequences. Clin Transpl 23:778–783
VanWagner LB, Skaro AI (2013) Program-specific reports: implications and impact on program behavior. Curr Opin Org Transplant 18:210–215
Adler NE, Newman K (2002) Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 21:60–76
Barrack RL, Ruh EL, Chen J, Lombardi AV Jr, Berend KR, Parvizi J, Della Valle CJ, Hamilton WG, Nunley RM (2014) Impact of socioeconomic factors on outcome of total knee arthroplasty. Clin Orthop Relat Res 472:86–97
Lasser KE, Himmelstein DU, Woolhandler S (2006) Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health 96:1300–1307
Schold JD, Phelan MP, Buccini LD (2017) Utility of ecological risk factors for evaluation of transplant center performance. Am J Transplant 17:617–621
Singh TP, Naftel DC, Addonizio L, Mahle W, Foushee MT, Zangwill S, Blume ED, Kirklin JK, Singh R, Johnston JK, Chinnock R (2010) Association of race and socioeconomic position with outcomes in pediatric heart transplant recipients. Am J Transplant 10:2116–2123
Evans JD, Kaptoge S, Caleyachetty R, Di Angelantonio E, Lewis C, Parameshwar KJ, Pettit SJ (2016) Socioeconomic deprivation and survival after heart transplantation in England: an analysis of the United Kingdom transplant registry. Circ Cardiovasc Qual Outcomes 9:695–703
Tumin D, Horan J, Shrider EA, Smith SA, Tobias JD, Jr HD, Foraker RE (2017) County socioeconomic characteristics and heart transplant outcomes in the United States. Am Heart J 190:104–112
Press R, Carrasquillo O, Nickolas T, Radhakrishnan J, Shea S, Barr RG (2005) Race/ethnicity, poverty status, and renal transplant outcomes. Transplantation 80:917–924
Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV (2005) Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the public health disparities geocoding project. Am J Public Health 95:312–323
United Network for Organ Sharing/Organ Procurement and Transplantation Network Data. Available at: https://optn.transplant.hrsa.gov/data—Accessed October 16, 2017
United States Census Bureau: American Community Survey Data. Available at: https://www.census.gov/programs-surveys/acs/data.html—Accessed October 16, 2017
Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL (2001) Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 345:99–106
Quillin RC 3rd, Wilson GC, Wima K, Hohmann SF, Sutton JM, Shaw JJ, Paquette IM, Woodle ES, Abbott DE, Shah SA (2014) Neighborhood level effects of socioeconomic status on liver transplant selection and recipient survival. Clin Gastroenterol Hepatol 12:1934–1941
Glance LG, Kellermann AL, Osler TM, Li Y, Li W, Dick AW (2016) Impact of risk adjustment for socioeconomic status on risk-adjusted surgical readmission rates. Ann Surg 263:698–704
Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM (2009) Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol 20:1333–1340
Schold JD, Heaphy EL, Buccini LD, Poggio ED, Srinivas TR, Goldfarb DA, Flechner SM, Rodrigue JR, Thornton JD, Sehgal AR (2013) Prominent impact of community risk factors on kidney transplant candidate processes and outcomes. Am J Transplant 13:2374–2383
Cao B, Adler JT, Bababekov YJ, Markmann JF, Chang DC, Yeh H (2018) Pediatric kidney transplantation and mortality: distance to transplant center matters. Pediatr Transplant. https://doi.org/10.1111/petr.13120
Begaj I, Khosla S, Ray D, Sharif A (2013) Socioeconomic deprivation is independently associated with mortality post kidney transplantation. Kidney Int 84:803–809
Stephens MR, Evans M, Ilham MA, Marsden A, Asderakis A (2010) The influence of socioeconomic deprivation on outcomes following renal transplantation in the United Kingdom. Am J Transplant 10:1605–1612
Ward FL, O’Kelly P, Donohue F, ÓhAiseadha C, Haase T, Pratschke J, deFreitas DG, Johnson H, Conlon PJ, O’Seaghdha CM (2015) Influence of socioeconomic status on allograft and patient survival following kidney transplantation. Nephrology (Carlton) 20:426–433
Aitken E, Dempster N, Ceresa C, Daly C, Kingsmore D (2013) The impact of socioeconomic deprivation on outcomes following renal transplantation in the West of Scotland. Transplant Proc 45:2176–2183
Laging M, Kal-van Gestel JA, van de Wetering J, IJzermans JN, Weimar W, Roodnat JI (2014) Understanding the influence of ethnicity and socioeconomic factors on graft and patient survival after kidney transplantation. Transplantation 98:974–978
Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R (2002) Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol 156:471–482
DeJong NA, Wood CT, Morreale MC, Ellis C, Davis D, Fernandez J, Steiner MJ (2016) Identifying social determinants of health and legal needs for children with special health care needs. Clin Pediatr (Phila) 55:272–277
Patel M, Bathory E, Scholnick J, White-Davis T, Choi J, Braganza S (2017) Resident documentation of social determinants of health: effects of a teaching tool in the outpatient setting. Clin Pediatr (Phila). https://doi.org/10.1177/000992281772869
Using social determinants of health data to improve health care and health: a learning report. Health Leads USA. Available at: https://healthleadsusa.org/wp-content/uploads/2016/06/RWJF-SDOH-Learning-Report.pdf—Accessed November 29, 2017
Screening for social determinants of health: two member experiences. Children’s Hospital Association. Available at: https://www.childrenshospitals.org/events/2016/04/14/screening-for-social-determinants-of-health-two-member-experiences—Accessed November 29, 2017
Peterson, EE (2017) Screening families for unmet social needs in a pediatric clinic. Wright State University
Isaacs R (2004) Ethical implications of ethnic disparities in chronic kidney disease and kidney transplantation. Adv Ren Replace Ther 11:55–58
Johansen KL, Zhang R, Huang Y, Patzer RE, Kutner NG (2012) Association of race and insurance type with delayed assessment for kidney transplantation among patients initiating dialysis in the United States. Clin J Am Soc Nephrol 7:1490–1497
Epstein AM, Ayanian JZ, Keogh JH, Noonan SJ, Armistead N, Clearly PD, Weissman JS, David-Kasdan JA, Carlson D, Fuller J, Marsh D, Conti RM (2000) Racial disparities in access to renal transplantation—clinically appropriate or due to underuse or overuse? N Engl J Med 343:1537–1544
Allmon AL, Shaw K, Martens JL, Yamada TH, Lohngberg JA, Schultz JM, Tallman BA, Altmaier EM (2010) Organ transplantation: issues in assessment and treatment. The Register Report
Laurentine KA, Bramstedt KA (2010) Too poor for transplant: finance and insurance issues in transplant ethics. Prog Transplant 20:178–185
Schaffer RL 3rd, Kulkarni S, Harper A, Millis JM, Cronin DC 2nd (2003) The sickest first? Disparities with model for end-stage liver disease-based organ allocation: one region’s experience. Liver Transpl 9:1211–1215
Trotter JF, Osgood MJ (2004) MELD scores of liver transplant recipients according to size of waiting list: impact of organ allocation and patient outcomes. JAMA 291:1871–1874
Barshes NR, Becker NS, Washburn WK, Halff GA, Aloia TA, Goss JA (2007) Geographic disparities in deceased donor liver transplantation within a single UNOS region. Liver Transpl 13:747–751
(1996) Pretending to be poor. The New York Times
Lieber R (2017) The ethics of adjusting your assets to qualify for Medicaid. The New York Times
(2005) Medicaid for millionaires. The Wall Street Journal
Tumin D, Foraker RE, Smith S, Tobias JD, Hayes D Jr (2016) Health insurance trajectories and long-term survival after heart transplantation. Circ Cardiovasc Qual Outcomes 9:576–584
Schlansky B, Shachar C (2016) Implications of expanded medicaid eligibility for patient outcomes after liver transplantation: Caveat emptor. Liver Transpl 22:1062–1064
Foraker RE, Tumin D, Smith S, Tobias JD, Hayes D Jr (2016) Insurance status by region at the time of heart transplantation: implications for survival. J Heart Lung Transplant 35:1480–1486
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Disclaimer
The data reported here have been supplied by the United Network for Organ Sharing as the contractor for the Organ Procurement and Transplantation Network (OPTN). The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the OPTN or the US Government.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Miller, R., Akateh, C., Thompson, N. et al. County socioeconomic characteristics and pediatric renal transplantation outcomes. Pediatr Nephrol 33, 1227–1234 (2018). https://doi.org/10.1007/s00467-018-3928-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-018-3928-0