Abstract
Background
Impairment in orexigenic/anorexigenic hormone balance may be key in the pathogenesis of protein energy wasting in children with chronic kidney disease (CKD). Measurement of ghrelin and obestatin concentrations in children with CKD would help assess the potential contribution of these hormones to uremic protein energy wasting.
Methods
This was a cross-sectional case–control study. Acylated and unacylated ghrelin and obestatin were measured in 42 children on conservative treatment (CT), 20 children on hemodialysis, 48 pediatric renal transplant (RTx) recipients and 43 controls (CTR) (mean age 11.9, range 5–20 years). Weight, height and bicipital, tricipital, subscapular and suprailiac folds were measured, and the body mass index-standard deviation score (BMI-SDS), percentage of fat mass and fat-free mass were calculated. Urea and creatinine were measured and the glomerular filtration rate (GFR) calculated.
Results
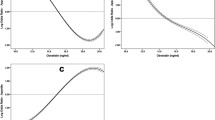
Unacylated ghrelin level was higher in patients than controls (p = 0.0001), with the highest levels found in hemodialysis patients (p = 0.001 vs. CKD-CT, p = 0.0001 vs. RTx, p < 0.0001 vs. CTR). Obestatin level was significantly higher in patients on hemodialysis than those on conservative treatment, RTx recipients and controls (p < 0.0001 in each case). Unacylated ghrelin negatively correlated with weight-SDS (p < 0.0001), BMI-SDS (p = 0.0005) and percentage fat mass (p = 0.004) and positively correlated with percentage fat-free mass (p = 0.004). Obestatin concentration negatively correlated with weight-SDS (p = 0.007). Unacylated ghrelin and obestatin concentrations positively correlated with creatinine and urea and inversely with eGFR, even after adjustments for gender, age, puberty and BMI-SDS (p < 0.0001 for each model).
Conclusions
Unacylated ghrelin and obestatin, negatively related to renal function, seem to be promising inverse indicators of nutritional status in children with CKD. Potential therapeutic implications in terms of optimization of their removal in patients on hemodialysis could be hypothesized.

Similar content being viewed by others
References
Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar-Zadeh K, Lochs H, Mantovani G, Marks D, Mitch WE, Muscaritoli M, Najand A, Ponikowski P, Rossi Fanelli F, Schambelan M, Schols A, Schuster M, Thomas D, Wolfe R, Anker SD (2008) Cachexia: a new definition. Clin Nutr 27:793–799
Mak RH, Ikizler AT, Kovesdy CP, Raj DS, Stenvinkel P, Kalantar-Zadeh K (2011) Wasting in chronic kidney disease. J Cachex Sarcopenia Muscle 2:9–25
Ulinski T, Cochat P (2006) Longitudinal growth in children following kidney transplantation: from conservative to pharmacological strategies. Pediatr Nephrol 21:903–909
Liu J, Prudom CE, Nass R, Pezzoli SS, Oliveri MC, Johnson ML, Veldhuis P, Gordon DA, Howard AD, Witcher DR, Geysen HM, Gaylinn BD, Thorner MO (2008) Novel ghrelin assays provide evidence for independent regulation of ghrelin acylation and secretion in healthy young men. J Clin Endocrinol Metab 93:1980–1987
Delhanty PJ, Neggers SJ, van der Lely AJ (2012) Mechanisms in endocrinology: Ghrelin: the differences between acyl- and des-acyl ghrelin. Eur J Endocrinol 167:601–608
Pradhan G, Samson SL, Sun Y (2013) Ghrelin: much more than a hunger hormone. Curr Opin Clin Nutr Metab Care 16:619–624
Zhang JV, Ren PG, Avsian-Kretchmer O, Luo CW, Rauch R, Klein C, Hsueh AJ (2005) Obestatin, a peptide encoded by the ghrelin gene, opposes ghrelin’s effects on food intake. Science 310:996–999
Trovato L, Gallo D, Settanni F, Gesmundo I, Ghigo E, Granata R (2014) Obestatin: is it really doing something? Front Horm Res 42:175–185
Pérez-Fontán M, Cordido F, Rodríguez-Carmona A, Peteiro J, García-Naveiro R, García-Buela J (2004) Plasma ghrelin levels in patients undergoing haemodialysis and peritoneal dialysis. Nephrol Dial Transplant 19:2095–2100
Iglesias P, Díez JJ, Fernández-Reyes MJ, Codoceo R, Alvarez-Fidalgo P, Bajo MA, Aguilera A, Selgas R (2006) Serum ghrelin concentrations in patients with chronic renal failure undergoing dialysis. Clin Endocrinol 64:68–73
Barazzoni R, Zanetti M, Stulle M, Mucci MP, Pirulli A, Dore F, Panzetta G, Vasile A, Biolo G, Guarnieri G (2008) Higher total ghrelin levels are associated with higher insulin-mediated glucose disposal in non-diabetic maintenance hemodialysis patients. Clin Nutr 27:142–149
Jarkovská Z, Hodková M, Sazamová M, Rosická M, Dusilová-Sulková S, Marek J, Justová V, Lacinová Z, Haluzík M, Haas T, Krsek M (2005) Plasma levels of active and total ghrelin in renal failure: a relationship with GH/IGF-I axis. Growth Hormon IGF Res 15:369–376
Yoshimoto A, Mori K, Sugawara A, Mukoyama M, Yahata K, Suganami T, Takaya K, Hosoda H, Kojima M, Kangawa K, Nakao K (2002) Plasma ghrelin and desacyl ghrelin concentrations in renal failure. J Am Soc Nephrol 13:2748–2752
Mafra D, Guebre-Egziabher F, Cleaud C, Arkouche W, Mialon A, Drai J, Fouque D (2010) Obestatin and ghrelin interplay in hemodialysis patients. Nutrition 26:1100–1104
Muscaritoli M, Molfino A, Chiappini MG, Laviano A, Ammann T, Spinsanti P, Melchiorri D, Inui A, Alegiani F, Rossi Fanelli F (2007) Anorexia in hemodialysis patients: the possible role of des-acyl ghrelin. Am J Nephrol 27:360–365
Büscher AK, Büscher R, Hauffa BP, Hoyer PF (2010) Alterations in appetite-regulating hormones influence protein-energy wasting in pediatric patients with chronic kidney disease. Pediatr Nephrol 25:2295–2301
Nüsken KD, Gröschl M, Rauh M, Stöhr W, Rascher W, Dötsch J (2004) Effect of renal failure and dialysis on circulating ghrelin concentration in children. Nephrol Dial Transplant 19:2156–2157
Arbeiter AK, Büscher R, Petersenn S, Hauffa BP, Mann K, Hoyer PF (2009) Ghrelin and other appetite-regulating hormones in paediatric patients with chronic renal failure during dialysis and following kidney transplantation. Nephrol Dial Transplant 24:643–646
Naufel MF, Bordon M, de Aquino TM, Ribeiro EB, de Abreu Carvalhaes JT (2010) Plasma levels of acylated and total ghrelin in pediatric patients with chronic kidney disease. Pediatr Nephrol 25:2477–2482
Aygen B, Dogukan A, Dursun FE, Aydin S, Kilic N, Sahpaz F, Celiker H (2009) Ghrelin and obestatin levels in end-stage renal disease. J Int Med Res 37:757–765
Borges N, Moraes C, Barros AF, Carraro-Eduardo JC, Fouque D, Mafra D (2014) Acyl-ghrelin and obestatin plasma levels in different stages of chronic kidney disease. J Ren Nutr 24:100–104
Lacquaniti A, Donato V, Chirico V, Pettinato G, Buemi M (2011) From chronic kidney disease to transplantation: the roles of obestatin. Regul Pept 171:48–52
Eftekhari MH, Ranjbar-Zahedani M, Basiratnia M, Rezaianzadeh A, Faghih S (2015) Comparison of appetite-regulating hormones and body composition in pediatric patients in predialysis stage of chronic kidney disease and healthy control group. Iran J Med Sci 40:27–33
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS, National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (2003) National Kidney Foundation’s kidney disease outcomes quality initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421
Cacciari E, Milani S, Balsamo A, Spada E, Bona G, Cavallo L, Cerutti F, Gargantini L, Greggio N, Tonini G, Cicognani A (2006) Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J Endocrinol Invest 29:581–593
Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 7:284–294
Siri WE (1961) Body composition from fluid spaces and density: analysis of methods. In: Brozek J, Henschel A (eds) Techniques for measuring body composition. National Academy of Sciences, Washington, DC, pp 223–224
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Alberti C, Chevenne D, Mercat I, Josserand E, Armoogum-Boizeau P, Tichet J, Léger J (2011) Serum concentrations of insulin-like growth factor (IGF)-1 and IGF binding protein-3 (IGFBP-3), IGF-1/IGFBP-3 ratio, and markers of bone turnover: reference values for French children and adolescents and z-score comparability with other references. Clin Chem 57:1424–1435
Crist W, Napier-Phillips A (2001) Mealtime behaviors of young children: a comparison of normative and clinical data. J Dev Behav Pediatr 22:279–286
Weir JB (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109:1–99
Harris JA, Benedict FG (1918) A biometric study of human basal metabolism. Proc Natl Acad Sci USA 4:370–373
Prodam F, Cadario F, Bellone S, Trovato L, Moia S, Pozzi E, Savastio S, Bona G (2014) Obestatin levels are associated with C-peptide and antiinsulin antibodies at the onset, whereas unacylated and acylated ghrelin levels are not predictive of long-term metabolic control in children with type 1 diabetes. J Clin Endocrinol Metab 99:E599–E607
Rodig NM, McDermott KC, Schneider MF, Hotchkiss HM, Yadin O, Seikaly MG, Furth SL, Warady BA (2014) Growth in children with chronic kidney disease: a report from the chronic kidney disease in children study. Pediatr Nephrol 29:1987–1995
Bonthuis M, van Stralen KJ, Verrina E, Groothoff JW, Alonso Melgar Á, Edefonti A, Fischbach M, Mendes P, Molchanova EA, Paripović D, Peco-Antic A, Printza N, Rees L, Rubik J, Stefanidis CJ, Sinha MD, Zagożdżon I, Jager KJ, Schaefer F (2013) Underweight, overweight and obesity in paediatric dialysis and renal transplant patients. Nephrol Dial Transplant 28:iv195–iv204
Johansen KL, Lee C (2015) Body composition in chronic kidney disease. Curr Opin Nephrol Hypertens 24:268–275
Haffner D, Zivicnjak M (2017) Pubertal development in children with chronic kidney disease. Pediatr Nephrol 32:949–964
Otto B, Tschöp M, Heldwein W, Pfeiffer AF, Diederich S (2004) Endogenous and exogenous glucocorticoids decrease plasma ghrelin in humans. Eur J Endocrinol 151:113–117
Gutierrez JA, Solenberg PJ, Perkins DR, Willency JA, Knierman MD, Jin Z, Witcher DR, Luo S, Onyia JE, Hale JE (2008) Ghrelin octanoylation mediated by an orphan lipid transferase. Proc Natl Acad Sci USA 105:6320–6325
De Vriese C, Hacquebard M, Gregoire F, Carpentier Y, Delporte C (2007) Ghrelin interacts with human plasma lipoproteins. Endocrinology 148:2355–2362
Gupta RK, Kuppusamy T, Patrie JT, Gaylinn B, Liu J, Thorner MO, Bolton WK (2013) Association of plasma des-acyl ghrelin levels with CKD. Clin J Am Soc Nephrol 8:1098–1105
Haqq AM, Farooqi IS, O’Rahilly S, Stadler DD, Rosenfeld RG, Pratt KL, LaFranchi SH, Purnell JQ (2003) Serum ghrelin levels are inversely correlated with body mass index, age, and insulin concentrations in normal children and are markedly increased in Prader–Willi syndrome. J Clin Endocrinol Metab 88:174–178
Prodam F, Monzani A, Ricotti R, Marolda A, Bellone S, Aimaretti G, Roccio M, Bona G (2014) Systematic review of ghrelin response to food intake in pediatric age, from neonates to adolescents. J Clin Endocrinol Metab 99:1556–1568
Rodriguez Ayala E, Pecoits-Filho R, Heimbürger O, Lindholm B, Nordfors L, Stenvinkel P (2004) Associations between plasma ghrelin levels and body composition in end-stage renal disease: a longitudinal study. Nephrol Dial Transplant 19:421–426
Foster-Schubert KE, Overduin J, Prudom CE, Liu J, Callahan HS, Gaylinn BD, Thorner MO, Cummings DE (2008) Acyl and total ghrelin are suppressed strongly by ingested proteins, weakly by lipids, and biphasically by carbohydrates. J Clin Endocrinol Metab 93:1971–1979
Wynne K, Giannitsopoulou K, Small CJ, Patterson M, Frost G, Ghatei MA, Brown EA, Bloom SR, Choi P (2005) Subcutaneous ghrelin enhances acute food intake in malnourished patients who receive maintenance peritoneal dialysis: a randomized, placebo-controlled trial. J Am Soc Nephrol 16:2111–2118
Ashby DR, Ford HE, Wynne KJ, Wren AM, Murphy KG, Busbridge M, Brown EA, Taube DH, Ghatei MA, Tam FW, Bloom SR, Choi P (2009) Sustained appetite improvement in malnourished dialysis patients by daily ghrelin treatment. Kidney Int 76:199–206
Rodríguez A, Gómez-Ambrosi J, Catalán V, Gil MJ, Becerril S, Sáinz N, Silva C, Salvador J, Colina I, Frühbeck G (2009) Acylated and desacyl ghrelin stimulate lipid accumulation in human visceral adipocytes. Int J Obes 33:541–552
Theander-Carrillo C, Wiedmer P, Cettour-Rose P, Nogueiras R, Perez-Tilve D, Pfluger P, Castaneda TR, Muzzin P, Schürmann A, Szanto I, Tschöp MH, Rohner-Jeanrenaud F (2006) Ghrelin action in the brain controls adipocyte metabolism. J Clin Invest 116:1983–1993
Temel JS, Abernethy AP, Currow DC, Friend J, Duus EM, Yan Y, Fearon KC (2016) Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol 17:519–531
Fischbach M, Zaloszyc A, Laetitia H, Menouer S, Terzic J (2014) Why does three times per week hemodialysis provide inadequate dialysis for children? Hemodial Int 18:S39–S42
Acknowledgements
The authors wish to thank the patients who took part to the study and all the medical and nursing staff of the Pediatric Nephrology, Dialysis and Transplant Unit of IRCCS Ca′ Granda–Ospedale Maggiore Policlinico, Milan, Italy. Special thanks to Dr. Maria Rosa Grassi, who performed the nutritional evaluations.
Sources of support
This study was supported by the charity organization “Associazione del bambino nefropatico”.
Author information
Authors and Affiliations
Contributions
AM, FlPr, GM and AE designed research; AM, MP, SM, ST and FaPa conducted research; AM, FlPr, GG and AR analyzed data; AM, GG, GB, GM and AE wrote the paper; AM had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
The study protocol was approved by the Ethics Committee of the Fondazione IRCCS Ca′ Granda–Ospedale Maggiore Policlinico, Milan, Italy (protocol number 396/2011 bis), and written informed consent was collected from the parents or legal guardians (and patients, where appropriate) of all children. All procedures were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Data
All data generated or analyzed during this study are included in this published article.
Additional information
This study is registered in the public trial registry www.clinicaltrials.com with the ID number NCT03171116.
Electronic supplementary material
ESM 1
(DOC 41 kb)
Rights and permissions
About this article
Cite this article
Monzani, A., Perrone, M., Prodam, F. et al. Unacylated ghrelin and obestatin: promising biomarkers of protein energy wasting in children with chronic kidney disease. Pediatr Nephrol 33, 661–672 (2018). https://doi.org/10.1007/s00467-017-3840-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3840-z