Abstract
Background
About half of children with steroid-sensitive idiopathic nephrotic syndrome (INS) will develop steroid dependency or a frequently relapsing course requiring steroid-sparing agents (SSA). Because of the adverse effects of prolonged steroid treatment, the early identification of children at high risk of requiring SSA may be a useful diagnostic tool to tailor the therapeutic strategy. The aim of this study was to identify predictors of the need for SSA and derive a predictive model.
Methods
This was a retrospective hospital-based cohort study which included all children with steroid-responsive INS followed for at least 4.5 months. Cox regression modeling and decision curve analysis were performed.
Results
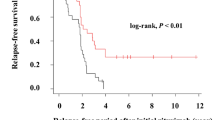
A total of 120 children (81 boys) with INS were included and followed up for a median time of 6.7 (range 0.4–24.1) years. Median age at diagnosis was 3.4 years. Seventy-two (60 %) children required a SSA after a median time of 10 months following initial diagnosis. Male children, age at disease onset, methylprednisolone pulse use, and time to achieve first remission were significantly associated with the outcome. Time to achieve remission only remained significant after adjustment: hazard ratio (HR) = 1.9 [95 % confidence interval (CI) 1.5–2.5] if considered as a continuous variable, and HR = 4.1 (95 % CI 1.9–8.6) when dichotomized using the 9-day threshold. The area under the receiver operating curve of the related predictive model was 0.81 (95 % CI 0.74–0.89), and the decision curve analysis demonstrated that this model performed better than any other strategy.
Conclusions
Time to first remission is a strong predictor of the need for SSA in pediatric INS. Further prospective and impact studies are warranted to confirm the accuracy and benefit of our prediction model.



Similar content being viewed by others
References
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639
[No authors listed] (1978) A report of the International Study of Kidney Disease in Children. Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. Kidney Int 13:159–165
Tarshish P, Tobin JN, Bernstein J, Edelmann CR Jr (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8:769–776
Hodson EM, Willis NS, Craig JC (2008) Non-corticosteroid treatment for nephrotic syndrome in children. Cochrane Database Syst Rev 1:CD002290
Barratt TM, Soothill JF (1970) Controlled trial of cyclophosphamide in steroid-sensitive relapsing nephrotic syndrome of childhood. Lancet 2:479–482
Latta K, von Schnakenburg C, Ehrich JH (2001) A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children. Pediatr Nephrol 16:271–282
British Association for Paediatric Nephrology (1991) Levamisole for corticosteroid-dependent nephrotic syndrome in childhood. Lancet 337:1555–1557
Ponticelli C, Edefonti A, Ghio L, Rizzoni G, Rinaldi S, Gusmano R, Lama G, Zacchello G, Confalonieri R, Altieri P, Bettinelli A, Maschio G, Cinotti GA, Fuiano G, Schena FP, Castellani A, Delia Casa-Alberighi O (1993) Cyclosporin versus cyclophosphamide for patients with steroid-dependent and frequently relapsing idiopathic nephrotic syndrome: a multicentre randomized controlled trial. Nephrol Dial Transplant 8:1326–1333
Hogg RJ, Fitzgibbons L, Bruick J, Bunke M, Ault B, Baqi N, Trachtman H, Swinford R (2006) Mycophenolate mofetil in children with frequently relapsing nephrotic syndrome: A report from the Southwest Pediatric Nephrology Study Group. Clin J Am Soc Nephrol 1:1173–1178
Guigonis V, Dallocchio A, Baudouin V, Dehennault M, Hachon-Le Camus C, Afanetti M, Groothoff J, Llanas B, Niaudet P, Nivet H, Raynaud N, Taque S, Ronco P, Bouissou F (2008) Rituximab treatment for severe steroid- or cyclosporine-dependent nephrotic syndrome: a multicentric series of 22 cases. Pediatr Nephrol 23:1269–1279
Constantinescu AR, Shah HB, Foote EF, Weiss LS (2000) Predicting first-year relapses in children with nephrotic syndrome. Pediatrics 105:492–495
Yap HK, Han EJ, Heng CK, Gong WK (2001) Risk factors for steroid dependency in children with idiopathic nephrotic syndrome. Pediatr Nephrol 16:1049–1052
Andersen RF, Thrane N, Noergaard K, Rytter L, Jespersen B, Rittig S (2010) Early age at debut is a predictor of steroid-dependent and frequent relapsing nephrotic syndrome. Pediatr Nephrol 25:1299–1304
Vivarelli M, Moscaritolo E, Tsalkidis A, Massella L, Emma F (2010) Time for initial response to steroids is a major prognostic factor in idiopathic nephrotic syndrome. J Pediatr 156:965–971
Letavernier B, Letavernier E, Leroy S, Baudet-Bonneville V, Bensman A, Ulinski T (2008) Prediction of high-degree steroid dependency in pediatric idiopathic nephrotic syndrome. Pediatr Nephrol 23:2221–2226
Bérard E, Broyer M, Dehennault M, Dumas R, Eckart P, Fischbach M, Loirat C, Martinat L, Pediatric Society of Nephrology (2005) Corticosensitive nephrotic syndrome (or nephrosis) in children. Therapeutic guideline proposed by the Pediatric Society of Nephrology. Nephrol Ther 1:150–156
Royston P, Altman DG, Sauerbrei W (2006) Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med 25:127
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 26:565–574
Niaudet P (2009) Long-term outcome of children with steroid-sensitive idiopathic nephrotic syndrome. Clin J Am Soc Nephrol 4:1547–1548
Rüth EM, Landolt MA, Neuhaus TJ, Kemper MJ (2004) Health-related quality of life and psychosocial adjustment in steroid-sensitive nephrotic syndrome. J Pediatr 145:778–783
Kabuki N, Okugawa T, Hayakawa H, Tomizawa S, Kasahara T, Uchiyama M (1998) Influence of age at onset on the outcome of steroid-sensitive nephrotic syndrome. Pediatr Nephrol 12:467–470
Fujinaga S, Hirano D, Nishizaki N (2011) Early identification of steroid dependency in Japanese children with steroid-sensitive nephrotic syndrome undergoing short-term initial steroid therapy. Pediatr Nephrol 26:485–486
MacHardy N, Miles PV, Massengill SF, Smoyer WE, Mahan JD, Greenbaum L, Massie S, Yao L, Nagaraj S, Lin JJ, Wigfall D, Trachtman H, Hu Y, Gipson DS (2009) Management patterns of childhood-onset nephrotic syndrome. Pediatr Nephrol 24:2193–2201
Ehrich JH, Brodehl J (1993) Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children. Arbeitsgemeinschaft für Pädiatrische Nephrologie. Eur J Pediatr 152:357–361
Hoyer PF, Brodehl J (2006) Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol 17:1151–1157
Funding
Sandrine Leroy was supported by a grant from the Fondation pour la Recherche Médicale and the French Foreign Office.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 44 kb)
Rights and permissions
About this article
Cite this article
Harambat, J., Godron, A., Ernould, S. et al. Prediction of steroid-sparing agent use in childhood idiopathic nephrotic syndrome. Pediatr Nephrol 28, 631–638 (2013). https://doi.org/10.1007/s00467-012-2365-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-012-2365-8