Abstract
Background
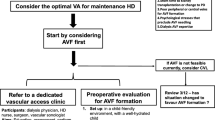
European and U.S. guidelines emphasise that permanent vascular access in the form of arteriovenous fistulae (AVF) or grafts (AVG) are preferable to central venous catheters (CVC) in paediatric patients on long-term haemodialysis. We report vascular access choice and complication rates in 13 European paediatric nephrology units.
Methods
A survey of units participating in the European Pediatric Dialysis Working Group requesting data on type of vascular access, routine care and complications in patients on chronic haemodialysis between March 2010 and February 2011.
Results
Information was complied on 111 patients in 13 participating centres with a median age of 14 (range 0.25–20.2) years. Central venous catheters were used in 67 of 111 (60%) patients, with 42 patients (38%) having an AVF and two patients (2%) having an AVG. Choice of vascular access was significantly related to patient age, with patients with AVF/AVG having a median age of 16 years compared to 12 years for patients with CVCs (p < 0.001). Routine CVC exit site care and catheter lock solution use differed between centres. CVC infections requiring intravenous antibiotics were reported at a rate of 1.9 and exit site infections at a rate of 1.8 episodes/1000 catheter days. Overall infective complications necessitating CVC change occurred at a rate of 0.9 episodes/1000 catheter days. No infective complications were reported in patients with AVF/AVG access. The rate of CVC infections requiring intravenous antibiotics was significantly lower in patients in whom CVC exit sites were cleaned weekly as opposed to every dialysis session (relative risk with every session cleaning vs. weekly cleaning 2.58, 95% confidence interval 1.17–5.69). Catheter malfunction (inadequate blood flow) was a more prevalent complication necessitating 22.4 thrombolytic interventions/1000 catheter days and 2.1 CVC changes/1000 catheter days.
Conclusions
Central venous catheters remain the predominant choice of vascular access in Europe despite problems of malfunction and infection. AVF/AVG were predominantly used in adolescents without reported complications. More regular exit site cleaning may predispose to CVC infection, but this observation requires prospective evaluation.




Similar content being viewed by others
References
Fischbach M, Edefonti A, Schroder C, Watson A, on behalf of the European Pediatric Dialysis Working Group (2005) Hemodialysis in children: general practical guidelines. Pediatr Nephrol 20:1054–1066
National Kidney Foundation (2006) National Kidney Foundation Disease Outcomes Quality Initiative: Clinical practice recommendations for vascular access. Available at: www.kidney.org/professionals/kdoqi
Chand DH, Valentini RP, Kamil ES (2009) Hemodialysis vascular access options in pediatrics: considerations for patients and practitioners. Pediatr Nephrol 24:1121–1128
NAPRTCs Annual Report (2011) Available at: http://www.emmes.com/study/ped/annlrept/annualrept2011.pdf
Fadrowski JJ, Hwang W, Neu AM, Fivush BA, Furth SL (2009) Patterns of use of vascular catheters for hemodialysis in children in the United States. Am J Kidney Dis 53:91–98
Mokrzycki MH, Lok CE (2010) Traditional and non-traditional strategies to optimize catheter function: go with more flow. Kidney Int 78:1218–1231
Stefanidis CJ (2010) Preventing catheter-related infections in children undergoing hemodialysis. Expert Rev Anti Infect Ther 8:1–11
Goldstein SL, Ikisler TA, Zappitelli M, Silverstein DM, Ayus JC (2009) Non-infected hemodialyis catheters are associated with increased inflammation compared to arteriovenous fistulas. Kidney Int 76:1063–1069
Lewis MA, Shaw J, Sinha MD, Adalat S, Hussain F, Castledine C, van Schalkwyk D, Inward C (2010) UK Renal Registry 12th Annual Report (December 2009): Chapter 14 Demography of the UK paediatric renal replacement therapy population in 2008. Nephron Clin Pract 115(Suppl1):c279–c288
Zaritsky JJ, Salusky AIB, Gales B, Ramos G, Atkinson J, Allsteadt A, Brandt ML, Goldstein SL (2008) Vascular access complications in long-term pediatric hemodialysis patients. Pediatr Nephrol 23:2061–2065
Chand DH, Valentini RP (2008) International pediatric fistula first initiative: a call to action. Am J Kidney Dis 51:1016–1024
Krishnamurthy G, Keller MS (2011) Vascular access in children. Cardiovasc interventional radiol 34:14–24
Bourquelot P, Raynaud F, Pirozzi N (2003) Microsurgery in children for creation of arteriovenous fistulas in renal and non-renal diseases. Ther Apher Dial 7:498–503
Astor BC, Eustace JA, Powe NR, Klag MJ, Sadler JH, Fink NE, Coresh J (2001) Timing of nephrologist referral and arteriovenous access use: the CHOICE Study. Am J Kidney Dis 38:494–501
Leonard MB, Donaldson LA, Ho M, Geary DF (2003) A prospective cohort study of incident maintenance dialysis in children: an NAPRTC study. Kidney Int 63:744–755
Male C, Chait P, Andrew M, Hanna K, Julian J, Mitchell L, for the PARKAA Investigators (2003) Central venous line-related thrombosis in children: association with central venous line location and insertion technique. Blood 101:4273–4278
Barrett N, Spencer S, McIovor J, Brown EA (1988) Subclavian stenosis: a major complication of subclavian dialysis catheters. Nephrol Dial Transpl 3:423–425
Agarwal AK, Patel BM, Haddad NJ (2007) Central venous stenosis: a nephrologist’s perspective. Semin Dial 20:53–62
Fischbach M, Terzic J, Laugel V, Dheu C, Menouer C, Helms P, Livolsi A (2004) Daily on-line haemodiafiltration: a pilot trial in children. Nephrol Dial Transpl 19:2360–2367
Fischbach M, Terzic J, Menouer C, Dheu C, Seuge L, Zalosczic A (2010) Daily on line haemodiafiltration promotes catch-up growth in children on chronic dialysis. Nephrol Dial Transpl 25:867–873
Sharma A, Zilleruelo G, Abitbol C, Montane B, Strauss J (1999) Survival and complications of cuffed catheters in children on chronic hemodialysis. Pediatr Nephrol 13:245–248
Sheth RD, Kale AS, Brewer ED, Brandt ML, Nuchtern JG, Goldstein SL (2001) Successful use of Tesio catheters in pediatric patients receiving chronic hemodialysis. Am J Kidney Dis 38:553–559
Ramage IJ, Bailie A, Tyerman KS, McColl JH, Pollard SG, Fitzpatrick MM (2005) Vascular access survival in children and young adults receiving long-term hemodialysis. Am J Kidney Dis 45:708–714
Fadel FI, Abdel Mooty HN, Bazaraa HM, Sabry SM (2008) Central venous catheters as a vascular access modality for pediatric hemodialysis. Int Urol Nephrol 40:489–496
Araya CE, Fennell RS, Neiberger RE, Dharnidharka VR (2007) Hemodialysis catheter-related bacteremia in children: increasing antibiotic resistance and changing bacteriological profile. Am J Kidney Dis 50:119–123
Peynircioglu B, Ozkan F, Canyigit M, Pamuk GA, Geyik S, Cil BE, Balkanci F (2007) Radiologically placed tunneled internal jugular catheters in the management of chronic hemodialysis and long-term infusion therapies in the pediatric population. J Vasc Interv Radiol 18:875–881
Onder AM, Chandar J, Billings A, Diaz R, Francoeur D, Abitbol C, Zilleruelo G (2009) Chlorhexidine-based antiseptic solutions effectively reduce catheter-related bacteremia. Pediatr Nephrol 24:1741–1747
Lok CE, Mokrzycki MH (2011) Prevention and management of catheter-related infection in hemodialysis patients. Kidney Int 79:587–598
Piraino B (2010) Dialysis: the importance of peritoneal catheter exit-site care. Nature Rev 6:259–260
Valentini RP, Geary DF, Chand DH (2008) Central venous lines for chronic hemodialysis: survey of the Midwest Pediatric Nephrology Consortium. Pediatr Nephrol 23:291–295
National Patient Safety Agency (2008) Risks with intravenous heparin flush solutions. NPSA/2008/444RRR002. Available at: www.npsa.nhs.uk/patientsafety
Gittins NS, Hunter-Blair YL, Matthews JNS, Coulthard MG (2007) Comparison of alteplase and heparin in maintaining the patency of paediatric central venous haemodialysis lines: a randomised controlled trial. Arch Dis Child 92:499–501
Hussain F, Connell R, Lunn A (2010) Alteplase (tPA) in pediatric hemodialysis (HD) patients—does it reduce catheter dysfunction, infections and the need for revisions? A prospective study. Pediatr Nephrol 25:1941
Hemmelgarn BR, Moist LM, Lok CE, Tonelli M, Manns BJ, Holden RM, LeBlanc M, Faris P, Barre P, Zhang J, Scott-Douglas N, for the Prevention of Dialysis Catheter Lumen Occlusion with rt-PA versus Heparin (PreCLOT) Study Group (2011) Prevention of dialysis catheter malfunction with recombinant tissue plasminogen activator. New Engl J Med 364:303–312
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The European Pediatric Dialysis Working Group comprises (in alphabetical order): Gema Ariceta, Pediatric Nephrology, Hospital Cruces, Barakaldo, Vizcaya, Spain; Sevcan A Bakkaloglu, Gazi University Hospital, Ankara, Turkey; Nichola Callaghan, Nottingham Children’s Hospital, Nottingham, UK (co-opted); Alberto Edefonti, Clinica Pediatrica De Marchi, Fondazione IRCCS Policlinico, Mangiagalli e Regina Elena, Milan, Italy; Mesiha Ekim, Ankara University Hospital, Ankara, Turkey; Michel Fischbach, Hopital de Hautepierre, Strasbourg, France; Wesley Hayes, Nottingham Children’s Hospital, Nottingham, UK (co-opted); Tuula Holtta, Children’s Hospital, University of Helsinki, Finland; Gunter Klaus, KfH Pediatric Kidney Center, Marburg, Germany; Claus Peter Schmitt, Center for Pediatric and Adolescent Medicine, Heidelberg, Germany; Rukshana Shroff, Great Ormond Street Hospital, London, UK; Constantinos J Stefanidis, “A & P Kyriakou” Children’s Hospital, Athens, Greece; Johan Van de Walle, University Hospital, Ghent, Belgium; Karen Vondrak, University Hospital Motol Prague, Czech Republic; Alan R Watson, Nottingham Children’s Hospital, Nottingham UK (Convenor); Elizabeth Wright, Great Ormond Street Hospital, London, UK (co-opted); Aleksandra Zurowska, Gdansk University Medical School, Poland
Rights and permissions
About this article
Cite this article
Hayes, W.N., Watson, A.R., Callaghan, N. et al. Vascular access: choice and complications in European paediatric haemodialysis units. Pediatr Nephrol 27, 999–1004 (2012). https://doi.org/10.1007/s00467-011-2079-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-011-2079-3