Abstract
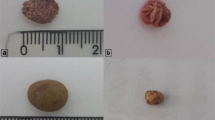
Although pediatricians are frequently confronted with patients presenting urolithiasis symptoms without obvious stones, the syndrome of occult urolithiasis may be still viewed with some skepticism. We have compared the clinical and metabolic features of 197 children with obvious calculi, 189 with microcalculi (diameter ≤3 mm based on renal sonography), and 114 with symptoms of urolithiasis and normal renal sonography findings. Only microcalculi and normal sonography subjects with a urinary abnormality potentially leading to urolithiasis were included in the study. Age at presentation increased significantly (p = 0.0001) in the groups in the order normal sonography to microcalculi to calculi groups. There was no significant difference among the three groups in terms of family history of urolithiasis, gender distribution, and degree of hypercalciuria, hyperuricosuria, hyperoxaluria, or hypocitraturia. The average frequency of pain attacks of patients with recurrent abdominal pain (RAP) ranged from 3.6 to 4.6 days of pain per month among the three groups, which is four to ninefold lower than that reported for children with functional or organic gastrointestinal RAP. The consistency of many clinical and urinary metabolic characteristics indicates a common underlying disorder in overt and occult urolithiasis. The increase of age at presentation from the normal sonography to microcalculi and calculi groups may reflect progressive crystal accretion leading ultimately to overt stone formation.

Similar content being viewed by others
References
Moore ES (1981) Hypercalciuria in children. Contr Nephrol 27:20–32
Heiliczer JD, Canonigo BB, Bishof NA, Moore ES (1987) Noncalculi Urinary Tract Disorders Secondary to Idiopathic Hypercalciuria in Children. Pediatr Clin North Am 34:711–717
Polito C, La Manna A, Cioce F, Villani J, Nappi B, Di Toro R (2000) Clinical presentation and natural course of idiopathic hypercalciuria in children. Pediatr Nephrol 15:211–214
Stapleton FB (1990) Idiopathic hypercalciuria: association with isolated hematuria and risk for urolithiasis in children. Kidney Int 37:807–811
Garcia CD, Miller LA, Stapleton FB (1991) Natural history of hematuria associated with hypercalciuria in children. Am J Dis Child 145:1204–1207
La Manna A, Polito C, Marte A, Iovene A, Di Toro R (2001) Hyperuricosuria in children: clinical presentation and natural history. Pediatrics 107:86–90
Cattini-Perrone H, Stapleton FB, Toporovsky J, Schor N (1997) Hematuria due to hyperuricosuria in children: 36-month follow-up. Clin Nephrol 48:288–291
Polito C, La Manna A, Signoriello G, Marte A (2009) Recurrent abdominal pains in childhood urolithiasis. Pediatrics 124:e1088–1094
Vachvanichsanong P, Malagon M, Moore ES (2001) Recurrent abdominal and flank pain in children with idiopathic hypercalciuria. Acta Paediatr 90:643–648
Hiorns MP (2008) Imaging of urinary tract lithiasis: who, when and how? Pediatr Radiol 38:S497–500
Manz F, Kehat R, Lausen B, Merkel A (1999) Urinary calcium excretion in healthy children and adolescents. Pediatr Nephrol 13:894–899
Alon U, Warady BA, Hellerstein S (1990) Hypercalciuria in the frequency-dysuria syndrome of childhood. J Pediatr 116:103–105
Escribano J, Balaguer A, Martin R, Feliu A, Espax R (2004) Childhood idiopathic hypercalciuria. Clinical significance of renal calyceal microlithiasis and risk of calcium nephrolithiasis. Scand J Urol Nephrol 38:422–426
Alpay H, Ozen A, Gokce I, Biyikli N (2009) Clinical and metabolic features of urolithiasis and microlithiasis in children. Pediatr Nephrol 24:2203–2209
Apley J, Naish N (1958) Recurrent abdominal pain: field survey of 1000 school children. Arch Dis Child 33:165–170
Miele E, Simeone D, Marino A, Greco L, Auricchio R, Novek SJ, Staiano A (2004) Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics 114:73–78
Ball TM, Weydert JA (2003) Methodological challenges to treatment trials for recurrent abdominal pain in children. Arch Pediatr Adolesc Med 157:1121–1127
Stordal K, Nygaard EA, Bentsen B (2001) Organic abnormalities in recurrent abdominal pain in children. Acta Paediatr 90:638–642
Alfvèn G (2003) One hundred cases of recurrent abdominal pain in children: diagnostic procedures and criteria for a psychosomatic diagnosis. Acta Paediatr 92:43–49
Srivastava T, Winston JM, Auron A, Alon US (2009) Urine calcium/citrate ratio in children with hypercalciuric stones. Pediatr Res 66:85–90
Bergstein J, Leiser J, Andreoli S (2005) The Clinical Significance of Asymptomatic Gross and Microscopic Hematuria in Children. Arch Pediatr Adolesc Med 159:353–355
Coward RJ, Peters CJ, Duffy PG, Corry P, Kellett MJ, Choong S, van’t Hoff WG (2003) Epidemiology of paediatric renal stone disease in the UK. Arch Dis Child 88:962–965
Gurgoze MK, Sari MY (2011) Results of medical treatment and metabolic risk factors in children withurolithiasis. Pediatr Nephrol 26:933–937
Curhan GC, Willett WC, Speizer FE, Rimm EB, Stampfer RJ (1997) Family history and risk of kidney stones. J Am Soc Nephrol 8:1568–1573
Weydert JA, Ball TM, Davis MF (2003) Systematic review of treatment for recurrent abdominal pain. Pediatrics 111:e1–11
Dursun I, Poyrazoglu HM, Dusunsel R, Gunduz Z, Gurgoze MK, Demizei D, Kucukaydin M (2008) Pediatric urolithiasis: an 8-year experience of single centre. Int Urol Nephrol 40:3–9
Pietrow PK, Pope JC, Adams MC, Shyr Y, Brock JW (2002) Clinical outcome of pediatric stone disease. J Urol 167:670–673
VanDervoort K, Wiesen J, Frank R, Vento S, Crosby V, Chandra M, Trachtman H (2007) Urolithiasis in pediatric patients: a single center study of incidence, clinical presentation and outcome. J Urol 177:2300–2305
Parks JH, Goldfisher E, Asplin JR, Coe FL (2002) A single 24-hour urine collection is inadequate for the medical evaluation of nephrolithiasis. J Urol 167:1607–1612
Alon US, Zimmerman H, Alon M (2004) Evaluation and treatment of pediatric idiopathic urolithiasis: revisited. Pediatr Nephrol 19:516–520
Stapleton FB (2005) Asymptomatic microscopic hematuria. Time to look the other way? Arch Pediatr Adolesc Med 159:398–399
Polito C, Marte A, La Manna A (2005) Appendectomy in children with hypercalciuria/hyperuricosuria. J Pediatr Urol 1:279–292
Castle SM, Cooperberg MR, Sadetsky N, Sadetsky N, Eisner BH, Stoller ML (2010) Adequacy of a single 24-hour urine collection for metabolic evaluation of recurrent nephrolithiasis. J Urol 184:579–583
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Polito, C., Apicella, A., Marte, A. et al. Clinical presentation and metabolic features of overt and occult urolithiasis. Pediatr Nephrol 27, 101–107 (2012). https://doi.org/10.1007/s00467-011-1940-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-011-1940-8