Abstract
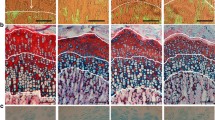
Growth retardation remains a major complication in children with primary tubular disorders, despite adequate supplemental treatment with electrolytes, water and bicarbonate. Chronic hypokalemia, characteristic of some tubulopathies, impairs growth by mechanisms that are not well known. Association with growth hormone deficiency has been reported in patients with Bartter’s or Gitelman’s syndrome. Tissue-specific alterations of growth hormone and insulin-like growth factor I axis have been described in experimental models of potassium depletion. Hypokalemic rats gain less body length and weight than pair-fed normokalemic animals and, by contrast, develop renal hypertrophy. These rats have low circulating concentrations of insulin-like growth factor I, depressed messenger ribonucleic acid (mRNA) levels of this peptide in the tibial growth plate, and they are resistant to the longitudinal growth-promoting effects of exogenous growth hormone. The reason for this resistance remains to be defined. No alterations in the intracellular signaling for growth hormone have been found in the liver of hypokalemic rats. However, treatment with high doses of growth hormone is unable to normalize hypertrophy of the epiphyseal cartilage chondrocytes, which are severely disturbed in potassium depletion and likely play an important role in the pathogenia of growth impairment in this condition.


Similar content being viewed by others
References
Haffner D, Weinfurth A, Manz F, Schmidt H, Bremer HJ, Mehls O, Schärer K (1999) Long-term outcome of paediatric patients with hereditary tubular disorders. Nephron 83:250–260
Haffner D, Weinfurth A, Seidel C, Manz F, Schmidt H, Waldherr R, Bremer HJ, Mehls O, Schärer K (1997) Body growth in primary de Toni-Debré-Fanconi syndrome. Pediatr Nephrol 11:40–45
Hsu SY, Tsai IJ, Tsau YK (2005) Comparison of growth in primary Fanconi syndrome and proximal renal tubular acidosis. Pediatr Nephrol 20:460–464
Greco M, Sesto A, Rizzoni G (1998) Body growth in primary de Toni-Debré-Fanconi syndrome. Pediatr Nephrol 12:83–84
McSherry E, Morris RC Jr (1978) Attainment and maintenance of normal stature with alkali therapy in infants and children with classic renal tubular acidosis. J Clin Invest 61:509–527
Rodriguez-Soriano J, Vallo A, Castillo G, Oliveros R (1982) Natural history of primary distal renal tubular acidosis treated since infancy. J Pediatr 101:669–676
Santos F, Chan JC (1986) Renal tubular acidosis in children. Diagnosis, treatment and prognosis. Am J Nephrol 6:289–295
Caldas A, Broyer M, Dechaux M, Kleinknecht C (1992) Primary distal tubular acidosis in childhood: clinical study and long-term follow-up of 28 patients. J Pediatr 121:233–241
Bajpai A, Bagga A, Hari P, Bardia A, Mantan M (2005) Long-term outcome in children with primary distal renal tubular acidosis. Indian Pediatr 42:321–328
Mitch WE, Medina R, Grieber S, May RC, England BK, Price SR, Bailey JL, Goldberg AL (1994) Metabolic acidosis stimulates muscle protein degradation by activating the adenosine triphosphate-dependent pathway involving ubiquitin and proteasomes. J Clin Invest 93:2127–2133
Ballmer PE, McNurlan MA, Hulter HN, Anderson SE, Garlick PJ, Krapf R (1995) Chronic metabolic acidosis decreases albumin synthesis and induces negative nitrogen balance in humans. J Clin Invest 95:39–45
Challa A, Krieg RJ Jr, Thabet MA, Veldhuis JD, Chan JC (1993) Metabolic acidosis inhibits growth hormone secretion in rats: mechanism of growth retardation. Am J Physiol 265:E547–E553
Ordóñez FA, Santos F, Martínez V, García E, Fernández P, Rodríguez J, Fernández M, Alvarez J, Ferrando S (2000) Resistance to growth hormone and insulin-like growth factor-I in acidotic rats. Pediatr Nephrol 14:720–725
Carbajo E, López JM, Santos F, Ordóñez FA, Niño P, Rodríguez J (2001) Histologic and dynamic changes induced by chronic metabolic acidosis in the rat growth plate. J Am Soc Nephrol 12:1228–1234
Bettinelli A, Bianchetti MG, Girardin E, Caringella A, Cecconi M, Appiani AC, Pavanello L, Gastaldi R, Isimbaldi C, Lama G, Marchesoni C, Matteucci C, Patriarca P, Di Natale B, Setzu C, Vitucci P (1992) Use of calcium excretion values to distinguish two forms of primary renal tubular hypokalemic alkalosis: Bartter and Gitelman syndromes. J Pediatr 120:38–43
Coto E, Rodriguez J, Jeck N, Alvarez V, Stone R, Loris C, Rodriguez LM, Fischbach M, Seyberth HW, Santos F (2004) A new mutation (intron 9 +1 G>T) in the SLC12A3 gene is linked to Gitelman syndrome in Gypsies. Kidney Int 65:25–29
Riveira-Munoz E, Chang Q, Godefroid N, Hoenderop JG, Bindels RJ, Dahan K, Devuyst O, Belgian Network for Study of Gitelman Syndrome (2007) Transcriptional and functional analyses of SLC12A3 mutations: new clues for the pathogenesis of Gitelman syndrome. J Am Soc Nephrol 18:1271–1283
Schurman SJ, Perlman SA, Sutphen R, Campos A, Garin EH, Cruz DN, Shoemaker LR (2001) Genotype/phenotype observations in African Americans with Bartter syndrome. J Pediatr 139:105–110
Bettinelli A, Borsa N, Bellantuono R, Syrèn ML, Calabrese R, Edefonti A, Komninos J, Santostefano M, Beccaria L, Pela I, Bianchetti MG, Tedeschi S (2007) Patients with biallelic mutations in the chloride channel gene CLCNKB: long-term management and outcome. Am J Kidney Dis 49:91–98
Seidel C, Reinalter S, Seyberth HW, Schärer K (1995) Pre-pubertal growth in the hyperprostaglandin E syndrome. Pediatr Nephrol 9:723–728
Vaisbich MH, Fujimura MD, Koch VH (2004) Bartter syndrome: benefits and side effects of long-term treatment. Pediatr Nephrol 19:858–863
Takahashi N, Chernavvsky DR, Gomez RA, Igarashi P, Gitelman HJ, Smithies O (2000) Uncompensated polyuria in a mouse model of Bartter’s syndrome. Proc Natl Acad Sci U S A 97:5434–5439
Lorenz JN, Baird NR, Judd LM, Noonan WT, Andringa A, Doetschman T, Manning PA, Liu LH, Miller ML, Shull GE (2002) Impaired renal NaCl absorption in mice lacking the ROMK potassium channel, a model for type II Bartter’s syndrome. J Biol Chem 277:37871–37880
Schultheis PJ, Lorenz JN, Meneton P, Nieman ML, Riddle TM, Flagella M, Duffy JJ, Doetschman T, Miller ML, Shull GE (1998) Phenotype resembling Gitelman’s syndrome in mice lacking the apical Na+-Cl- cotransporter of the distal convoluted tubule. J Biol Chem 273:29150–29155
Requeira O, Rao J, Baliga R (1991) Response to growth hormone in a child with Bartter’s syndrome. Pediatr Nephrol 5:671–672
Ko CW, Koo JH (1999) Recombinant human growth hormone and Gitelman’s syndrome. Am J Kidney Dis 33:778–781
Itami N, Satake N, Yoshida M, Ohshika E, Koga Y (1992) Bartter’s syndrome and growth hormone replacement. Lancet 340:1406–1407
Boer LA, Zoppi G (1992) Bartter’s syndrome with impairment of growth hormone secretion. Lancet 340:860
Ruvalcaba RH, Martinez FE (1992) Case report: familial growth hormone deficiency associated with Bartter’s syndrome. Am J Med Sci 303:411–414
Bettinelli A, Rusconi R, Ciarmatori S, Righini V, Zammarchi E, Donati MA, Isimbaldi C, Bevilacqua M, Cesareo L, Tedeschi S, Garavaglia R, Casari G (1999) Gitelman disease associated with growth hormone deficiency, disturbances in vasopressin secretion and empty sella: a new hereditary renal tubular-pituitary syndrome? Pediatr Res 46:232–238
Flyvbjerg A, Dørup I, Everts ME, Orskov H (1991) Evidence that potassium deficiency induces growth retardation through reduced circulating levels of growth hormone and insulin-like growth factor I. Metabolism 40:769–775
Dørup I, Flyvbjerg A (1993) Effects of IGF-I infusion on growth and muscle Na(+)-K+ pump concentration in K(+)-deficient rats. Am J Physiol 264:E810–E815
Hochberg Z, Amit T, Flyvbjerg A, Dørup I (1995) Growth hormone (GH) receptor and GH-binding protein deficiency in the growth failure of potassium-depleted rats. J Endocrinol 147:253–258
van Neck JW, Flyvbjerg A, Schuller AG, Rosato RR, Groffen C, van Kleffens M, Lindenbergh-Kortleve D, Dørup I, Drop SL (1997) IGF, type I IGF receptor and IGF-binding protein mRNA expression in kidney and liver of potassium-depleted and normal rats infused with IGF-I. J Mol Endocrinol 19:59–66
Hsu FW, Tsao T, Rabkin R (1997) The IGF-I axis in kidney and skeletal muscle of potassium deficient rats. Kidney Int 52:363–370
Schaefer F, Yoon SA, Nouri P, Tsao T, Tummala P, Deng E, Rabkin R (2004) Growth hormone-mediated janus associated kinase-signal transducers and activators of transcription signaling in the growth hormone-resistant potassium-deficient rat. J Am Soc Nephrol 15:2299–3306
Gil-Peña H, Garcia-Lopez E, Alvarez-Garcia O, Loredo V, Carbajo-Perez E, Ordoñez FA, Rodriguez-Suarez J, Santos F (2009) Alterations of growth plate and abnormal insulin-like growth factor I metabolism in growth-retarded hypokalemic rats: effect of growth hormone treatment. Am J Physiol Renal Physiol 297:F639–F645
Acknowledgments
This work was supported by grant FIS 06/1730 and Fundación Nutrición y Crecimiento. It was completed during the sabbatical stay of N. Mejia from Hospital Universitario Fundación Santa Fé, Bogotá, Colombia. Presented in part at the 8th International Symposium on Growth and Nutrition in Children with Chronic Renal Disease, Oviedo, Spain, 28–30 May 2009.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gil-Peña, H., Mejia, N., Alvarez-Garcia, O. et al. Longitudinal growth in chronic hypokalemic disorders. Pediatr Nephrol 25, 733–737 (2010). https://doi.org/10.1007/s00467-009-1330-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1330-7