Abstract
Proteomic analysis has revealed potential early biomarkers of acute kidney injury (AKI) in children undergoing cardiopulmonary bypass (CPB), the most prominent one with a mass-to-charge ratio of 6.4 kDa. The objective of this study was to identify this protein and test its utility as a biomarker of AKI. Trypsin-digested protein bands were analyzed by tandem mass spectrometry (MS/MS) to identify the protein in urine samples. Surface-enhanced laser desorption/ionization time-of-flight analysis and a functional activity assay were performed to quantify urinary levels in a pilot study of 106 pediatric patients undergoing CPB. The protein was identified as aprotinin. Urinary aprotinin levels 2 h after initiation of CPB were predictive of AKI (for functional assay: 92% sensitivity, 96% specificity, area under the curve of 0.98). By multivariate analysis, the urinary aprotinin level 2 h after CPB was an independent predictor of AKI (β = 0.001, P < 0.0001). The 2 h urinary aprotinin level correlated with serum creatinine, duration of AKI, and length of hospital stay. We concluded that urinary aprotinin levels 2 h after initiation of CPB predict the development of AKI and adverse clinical outcomes.


Similar content being viewed by others
References
Albert MA, Antman EM (2003) Preoperative evaluation for cardiac surgery. In: Cohn LH, Edmunds LH Jr (eds) Cardiac surgery in the adult. New York, McGraw-Hill, pp 235–248
Haase M, Haase-Fielitz A, Bagshaw SM, Ronco C, Bellomo R (2007) Cardiopulmonary bypass-associated acute kidney injury: a pigment nephropathy? Contrib Nephrol 156:340–353
Rosner MH, Okusa MD (2006) Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol 1:19–32
Chertow GM, Levy EM, Hammermeister KE, Grover F, Daley J (1998) Independent association between acute renal failure and mortality following cardiac surgery. Am J Med 104:343–348
Lassning A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M (2004) Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 15:1597–1605
Thakar CV, Worley S, Arrigain S, Yared J-P, Paganini EP (2005) Influence of renal dysfunction on mortality after cardiac surgery: modifying effect of preoperative renal function. Kidney Int 67:1112–1119
Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT (1998) Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med 128:194–203
Lok CE, Austin PC, Wanh H, Tu JV (2004) Impact of renal insufficiency on short- and long-term outcomes after cardiac surgery. Am Heart J 148:430–438
Loef BG, Epema AH, Smilde TB, Henning RH, Ebels T, Navis G, Stegemean CA (2005) Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J Am Soc Nephrol 16:195–200
Sorof JM, Stromberg D, Brewer ED, Feltes TF, Fraser CD Jr (1999) Early initiation of peritoneal dialysis after surgical repair of congenital heart disease. Pediatr Nephrol 13:641–645
Mehta RL (2005) Acute renal failure and cardiac surgery: marching in place or moving ahead? J Am Soc Nephrol 16:12–14
Thakar CV, Arrigain S, Worley S, Yared J-P, Paganini EP (2005) A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol 16:162–168
Mehta RH, Grab JD, O’Brien SM, Bridges CR, Gammie JS, Haan CK, Ferguson TB, Peterson ED, the Society of Thoracic Surgeons National Cardiac Surgery Database Investigators (2006) Bedside tool for predicting the risk of postoperative dialysis in patients undergoing cardiac surgery. Circulation 114:2208–2216
Wijeysundera DN, Karkouti K, Dupuis JY, Rao V, Chan CT, Granton JT, Beattie WS (2007) Derivation and validation of a simplified predictive index for renal replacement therapy after cardiac surgery. JAMA 297:1801–1809
Devarajan P (2006) Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol 17:1503–1520
Jo SK, Rosner MH, Okusa MD (2007) Pharmacologic treatment of acute kidney injury: why drugs haven’t worked and what is on the horizon. Clin J Am Soc Nephrol 2:356–365
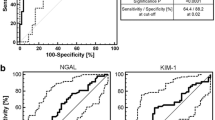
Mishra J, Dent C, Tarabishi R, Mitsnefes MM, Ma Q, Kelly C, Ruff SM, Zahedi K, Shao M, Bean J, Mori K, Barasch J, Devarajan P (2005) Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet 365:1231–1238
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Concensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 8:R204–R212
Nguyen MT, Ross GF, Dent CL, Devarajan P (2005) Early prediction of acute renal injury using urinary proteomics. Am J Nephrol 25:318–326
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI (2002) Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 123:110–118
Wernovsky G, Wypij D, Jonas RA, Mayer JE Jr, Hanley FL, Hickey PR, Walsh AZ, Chang AC, Castaneda AR, Newburger JW, Wessel DL (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants: a comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92:2226–2235
Kulik TJ, Moler FW, Palmisano JM, Custer JR, Mosca RS, Bove EL, Bartlett RH (1996) Outcome-associated factors in pediatric patients treated with extracorporeal membrane oxygenator after cardiac surgery. Circulation 94 [Suppl II]:63–68
Cardigan RA, Mackie IJ, Gippner-Steppert C, Jochum M, Royston D, Gallimore MJ (2001) Determination of plasma aprotinin levels by functional and immunologic assays. Blood Coagul Fibrinolysis 12:37–42
Devarajan P (2007) Emerging biomarkers of acute kidney injury. Contrib Nephrol 156:203–212
Royston D, van Haaften N, De Vooght P (2007) Aprotinin; friend or foe? A review of recent medical literature. Eur J Anaesthesiol 24:6–14
Henry DA, Moxey AJ, Carless PA, O’Connell D, McClelland B, Henderson KM, Sly K, Laupacis A, Fergusson D (2001) Anti-fibrinolytic use for minimizing perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 1:CD001886
Sedrakyan A, Treasure T, Elefteriades JA (2004) Effect of aprotinin on clinical outcomes in coronary artery bypass graft surgery: a systematic review and meta-analysis of randomized clinical trials. J Thorac Cardiovasc Surg 128:442–448
Fauli A, Gomar C, Campistol JM, Alvarez L, Manig AM, Matute P (2005) Kidney-specific proteins in patients receiving aprotinin at high- and low-dose regimens during coronary artery bypass graft with cardiopulmonary bypass. Eur J Anaesthesiol 22:666–671
Karkouti K, Beattie WS, Dattilo KM, McCluskey SA, Ghannam M, Hamdy A, Wijeysundara DM, Fedorko L, Yau TM (2006) A propensity score case-control comparison of aprotinin and tranexamic acid in high-transfusion-risk cardiac surgery. Transfusion 46:327–338
Mangano DT, Tudor IC, Dietzel C (2006) The risk associated with aprotinin in cardiac surgery. N Engl J Med 354:353–365
Mangano DT, Miao Y, Vuylsteke A, Tudor IC, Juneja R, Filipescu D, Hoeft A, Fontes ML, Hillel Z, Ott E, Titov T, Dietzel C, Levin J (2007) Mortality associated with aprotinin during 5 years following coronary artery bypass graft surgery. JAMA 297:471–479
Hunter D (2006) First, gather the data. N Engl J Med 354:329–331
Vlahakes GJ (2006) The value of phase 4 clinical testing. N Engl J Med 354:413–415
Ferraris VA, Bridges CR, Anderson RP (2006) Aprotinin in cardiac surgery. N Engl J Med 354:1953–1954
Levy JH, Ramsay JG, Guyton RA (2006) Aprotinin in cardiac surgery. N Engl J Med 354:1956
D’Ambra MN (2006) Aprotinin in cardiac surgery. N Engl J Med 354:1956
Brown J, Birkmeyer N, O’Connor J (2006) Aprotinin in cardiac surgery. N Engl J Med 354:1954–1955
Rieves RD, Weiss KD (2006) Aprotinin in cardiac surgery. N Engl J Med 355:2262
Acknowledgments
Prasad Devarajan is supported by grants from the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NIDDK) (RO1 DK069749, RO1 HL08676). Mai Nguyen is supported by a Fellowship grant from the American Heart Association. We are grateful to Drs. Thomas J. Kulik, Bradley S. Marino and Arnold W. Strauss for their critical review of the manuscript. We are indebted to our nurse coordinators, Tracey VanVliet, Lois Bogenshutz, Teresa Barnard, and Kristen Buschle, for their assistance, and to our patients and their families for their participation.
Conflict of interest statement
The authors declare that they have no conflict of interest related to the contents of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Mai T. Nguyen and Catherine L. Dent contributed equally to this work.
Rights and permissions
About this article
Cite this article
Nguyen, M.T., Dent, C.L., Ross, G.F. et al. Urinary aprotinin as a predictor of acute kidney injury after cardiac surgery in children receiving aprotinin therapy. Pediatr Nephrol 23, 1317–1326 (2008). https://doi.org/10.1007/s00467-008-0827-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-0827-9