Abstract
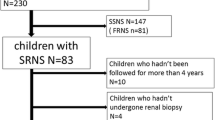
Childhood nephrotic syndrome (NS) is frequently characterized by a relapsing course. There is no uniform agreement about the precise stage at which a steroid-sparing agent should be introduced to control the disease. In order to evaluate the treatment strategies and outcome of steroid-sensitive NS over the last 2 decades, a retrospective notes review was undertaken in a cohort of children treated at Great Ormond Street Children's Hospital between 1980 and 2000. From a population of 863 children with NS referred, 509 had frequently relapsing or steroid-dependent disease and 261 children received at least one steroid-sparing agent. Cyclophosphamide was the first choice in 178 patients and in 114 no further steroid-sparing agent was needed. Levamisole was prescribed as the first steroid-sparing agent for 65 children and disease control was achieved in 30%. Cyclosporin A was prescribed in 61 children and sustained remission was induced in 69%. It is concluded that cyclophosphamide is a potent agent in inducing sustained remission in steroid-sensitive NS. Levamisole and cyclosporin A have emerged as attractive steroid-sparing agents. Complications and major side effects of treatment are infrequent but occasionally fatal.


Similar content being viewed by others
References
Koskimes O (1982) Long term outlook of primary nephrotic syndrome. Arch Dis Child 57:544–548
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS (1985) Long-term outcome for children with minimal change nephrotic syndrome. Lancet I:368–370
Hoyer PF, Gonda S, Barthels M, Krohn HP, Brodehl J (1986) Thromboembolic complications in children with nephrotic syndrome. Risk and incidence. Acta Paediatr Scand 75:804–807
Kresnsky AM, Ingelfinger JR, Grupe WE (1982) Peritonitis in childhood nephrotic syndrome. Am J Dis Child 136:732–736
Ehrich JH, Brodehl J (1993) Long versus standard prednisone therapy for initial treatment of idiopathic nephrotic syndrome in children (Arbeitsgemeinschaft für Pädiatrische Nephrologie). Eur J Pediatr 150:380–387
Brodehl J (1991) Conventional therapy for idiopathic nephrotic syndrome in children. Clin Nephrol 35 [Suppl 1]:S8–S15
Trompeter RS (1989) Immunosuppressive therapy in nephrotic syndrome in children. Pediatr Nephrol 3:218–220
Latta K, Schnakenburg C von, Ehrich JH (2001) A meta-analysis of cytotoxic treatment for frequently relapsing nephrotic syndrome in children Pediatr Nephrol 16:271–282
Consensus statement on management and audit potential for steroid responsive nephrotic syndrome (1994) Report of a workshop by the British Association for Paediatric Nephrology and Research Unit, Royal College of Physicians. Arch Dis Child 70:151–157
Neuhaus TJ, Fay J, Dillon MJ, Trompeter RS, Barratt TM (1994) Alternative treatment to corticosteroids in steroid sensitive idiopathic nephrotic syndrome. Arch Dis Child 71:522–526
Trompeter RS (1986) Minimal change nephrotic syndrome and cyclophosphamide. Arch Dis Child 61:727–729
International Study of Kidney Disease in Children (1982) Early identification of frequent relapsers among children with minimal change nephrotic syndrome. J Pediatr 101:514–518
Bouissou F, Meissner I, Konrad M, Sommer E, Mytilineos J, Ohayon E, Sierp G, Barthe B, Opelz G, Cambon-Thomsen A, et al (1995) Clinical implications from studies of HLA antigens in idiopathic nephrotic syndrome in children. Clin Nephrol 44:279–283
Zidar N, Avgustin CM, Kenda RB, Ferluga D (1998) Unfavorable course of minimal change nephrotic syndrome in children with intrauterine growth retardation Kidney Int 54:1320–1323
Kabuki N, Okugawa T, Hayakawa H, Tomizawa S, Kasahara T, Uchiyama M (1998) Influence of age at onset on the outcome of steroid-sensitive nephrotic syndrome. Pediatr Nephrol 12:467–470
Shalhoub RJ (1974) Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet II:556–560
Hulton SA, Shah V, Byrne MR, Morgan G, Barratt TM, Dillon MJ (1994) Lymphocyte subpopulations, interleukin-2 and interleukin-2 receptor expression in childhood nephrotic syndrome. Pediatr Nephrol 8:135–139
Topaloglu R, Saatci U, Arikan M, Canpinar H, Bakkaloglu A, Kansu E (1994) T-cell subsets, interleukin-2 receptor expression and production of interleukin-2 in minimal change nephrotic syndrome. Pediatr Nephrol 8:649–652
Trompeter RS, Layward L, Hayward AR (1978) Primary and secondary abnormalities of T cell sub populations. Clin Exp Immunol 34:388–392
Yap H, Cheung W, Murugasu M, Sim S, Seah C Jordon SC (1999) Th1 and Th2 cytokine mRNA profiles in childhood nephrotic syndrome: evidence for increased IL-13 mRNA expression in relapse. J Am Soc Nephrol 10:529–537
Durkan AM, Hodson EM, Willis NS, Craig JC (2001) Immunosuppressive agents in childhood nephrotic syndrome: a meta-analysis of randomised controlled trials. Kidney Int 59:1919–1927
Barratt TM, Bercowsky A, Osofsky SG, Soothill JF (1975) Cyclophosphamide treatment in steroid-sensitive nephrotic syndrome of childhood. Lancet 1:55–58
Etteldorf JN, West CD, Pitcock JA, Williams DL (1976) Gonadal function, testicular histology, and meiosis following cyclophosphamide therapy in patients with nephrotic syndrome. J Pediatr 88:206–212
Fu LS, Chi CS (2000) Levamisole in steroid-sensitive nephrotic syndrome children with steroid-dependency and/or frequent relapses. Acta Paediatr Taiwan 41:80–84
British Association for Paediatric Nephrology (1991) Levamisole for corticosteroid-dependent nephrotic syndrome in childhood. . Lancet 337:1555–1557
Bagga A, Hari P (2000) Levamisole-induced vasculitis. Pediatr Nephrol 14:1057–1058
Bulugahapitiya DT (1997) Liver toxicity in a nephrotic patient treated with levamisole. Arch Dis Child 76:289
Ginevri F, Trivelli A, Ciardi MR, Ghiggeri GM, Parfumo F, Gusmano R (1996) Protracted levamisole in children with frequent-relapse nephrotic syndrome. Pediatr Nephrol 10:550
Brodehl J (1996) Management of nephrotic syndrome in children. Clin Immunother 5:175–192
Bia MJ, Flye W (1984) Lymphoma and cyclosporin. Lancet I:1408
Walker RJ, Tiller DJ, Horvath JS, Duggin GG (1989) Malignant lymphoma in a renal transplant patient on cyclosporin A therapy. Aust N Z J Med 19:154–155
Grupe WE, Makker SP, Ingelfinger JR (1976) Chlorambucil treatment of frequently relapsing nephrotic syndrome. N Engl J Med 295:746–749
Mees EJH (1996) Does it make sense to administer albumin to the patient with nephrotic oedema. Nephrol Dial Transplant 11:1224–1225
Haws RM, Baum M (1993) Efficacy of albumin and diuretic therapy in children with nephrotic syndrome. Pediatrics 91:1142–1146
Acknowledgements
A.A. was supported by The Caring for Kids Fund (Child Health Research Appeal Trust).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abeyagunawardena, A.S., Dillon, M.J., Rees, L. et al. The use of steroid-sparing agents in steroid-sensitive nephrotic syndrome. Pediatr Nephrol 18, 919–924 (2003). https://doi.org/10.1007/s00467-003-1216-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1216-z