Abstract
Introduction
The use of bioabsorbable mesh at the hiatus is controversial. Long-term data are scant. We evaluated the world literature and performed a meta-analysis to determine if these meshes were effective in reducing recurrence.
Methods
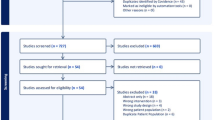
A literature search was performed using PubMed, MEDLINE, and ClinicalKey. We evaluated articles reporting on both Bio-A™ (polyglycolic acid:trimethylene carbonate—PGA:TMC) and Phasix™ (poly-4-hydroxybutyrate—P4HB) used at the hiatus. The DerSimonian–Laird random effects model was used to estimate the overall pooled treatment effect along with a 95% confidence interval (CI). Similar analysis was conducted to compare the clinical outcomes, i.e., recurrence rate, mean surgical time, mean hospital stays and mean follow-up duration between non-Mesh and Mesh group. The I2 statistic was computed to assess the heterogeneity in effect sizes across the studies.
Results
A total of 21 studies (12 mesh studies with 963 subjects and 9 non-mesh studies with 617 subjects) were included to conduct the meta-analysis. There was one article reporting outcomes on P4HB mesh (73 subjects) and 11 on PGA:TMC mesh (890 subjects). The bioabsorbable mesh group had a significantly lower recurrence rate compared to the non-mesh group (8% vs. 18%; 95%CI 0.08−0.17), pooled p-value < 0.0001. Surgery time was shorter in the mesh group compared to the non-mesh group (136.4 min vs. 150 min) but not statistically significant (p = 0.54). There tended to be a more extended follow-up period after surgery in the non-mesh group compared to the mesh group (27 vs. 25.8 months, range 10.8–54 months); but not statistically significant (ES: 27.4; 95%CI 21.6−33.3; p = 0.92).
Conclusions
Hiatal hernia repair with bioabsorbable mesh is more effective at reducing hernia recurrence rate in the mid-term than simple suture cruroplasty. Further studies investigating the long-term outcomes and P4HB mesh are needed.





Similar content being viewed by others
References
Dallemagne B, Kohnen L, Perretta S, Weerts J, Markiewicz S, Jehaes C (2011) Laparoscopic repair of paraesophageal hernia. Long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg. https://doi.org/10.1097/SLA.0b013e3181ff44c0
Dubina ED, Moazzez A, Park H, Shover A, Kim DY, Simms ER (2019) Predictors of morbidity and mortality in complex paraesophageal hernia repair: A NSQIP analysis. Am Surg 85(10):1189–1193
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA (2012) Lower recurrence rates after mesh-reinforced versus simple hiatal hernia repair: a meta-analysis of randomized trials. Surg Laparosc Endosc Percutan Tech 22(6):498–502. https://doi.org/10.1097/SLE.0b013e3182747ac2
Andujar JJ, Papasavas PK, Birdas T, Robke J, Raftopoulos Y, Gagné DJ, Caushaj PF, Landreneau RJ, Keenan RJ (2004) Laparoscopic repair of large paraesophageal hernia is associated with a low incidence of recurrence and reoperation. Surg Endosc 18(3):444–447. https://doi.org/10.1007/s00464-003-8823-4
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240(4):578–583. https://doi.org/10.1097/01.sla.0000141193.08524.e7
Armijo PR, Krause C, Xu T, Shostrom V, Oleynikov D (2021) Surgical and clinical outcomes comparison of mesh usage in laparoscopic hiatal hernia repair. Surg Endosc 35(6):2724–2730. https://doi.org/10.1007/s00464-020-07703-4
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG, Demeester TR, Swanstrom LL, Daniel Smith C, Filipi CJ (2009) Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23(6):1219–1226. https://doi.org/10.1007/s00464-008-0205-5
Watson DI, Thompson SK, Devitt PG, Smith L, Woods SD, Aly A, Gan S, Game PA, Jamieson GG (2015) Laparoscopic repair of very large hiatus hernia with sutures versus absorbable mesh versus nonabsorbable mesh: a randomized controlled trial. Ann Surg 261(2):282–289. https://doi.org/10.1097/SLA.0000000000000842
Alicuben ET, Worrell SG, DeMeester SR (2014) Resorbable biosynthetic mesh for crural reinforcement during hiatal hernia repair. Am Surg 80(10):1030–1033. https://doi.org/10.1177/000313481408001026
Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, Polissar NL, Neradilek MB, Mitsumori LM, Rohrmann CA, Swanstrom LL (2011) Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg 213(4):461–468. https://doi.org/10.1016/j.jamcollsurg.2011.05.017
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J, Swanstrom L (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244(4):481–490. https://doi.org/10.1097/01.sla.0000237759.42831.03
Inaba CS, Oelschlager BK, Yates RB, Khandelwal S, Chen JY, Wright AS (2022) Characteristics and outcomes of patients undergoing paraesophageal hernia repair with selective use of biologic mesh. Surg Endosc 36(2):1627–1632. https://doi.org/10.1007/s00464-021-08399-w
BioA (2022) GORE® BIO-A® Tissue Reinforcement. https://www.goremedical.com/products/bioatissue. Accessed 12 Mar 2022
Phasix™ Mesh (2022) Fully resorbable implant for soft tissue reconstruction. https://www.bd.com/en-us/products-and-solutions/products/product-families/phasix-mesh. Accessed 12 Mar 2022
Olson MT, Mittal SK, Bremner RM (2021) A collective review of gore bio-a absorbable synthetic mesh in cruroplasty reinforcement. J Laparoendosc Adv Surg Tech A 31(1):61–70. https://doi.org/10.1089/lap.2020.0343
Abdelmoaty WF, Dunst CM, Filicori F, Zihni AM, Davila-Bradley D, Reavis KM, Swanstrom LL, DeMeester SR (2020) Combination of surgical technique and bioresorbable mesh reinforcement of the Crural repair leads to low early hernia recurrence rates with laparoscopic paraesophageal hernia repair. J Gastrointest Surg 24(7):1477–1481. https://doi.org/10.1007/s11605-019-04358-y
FitzGerald JF, Kumar AS (2014) Biologic versus synthetic mesh reinforcement: what are the pros and cons? Clin Colon Rectal Surg 27(4):140–148. https://doi.org/10.1055/s-0034-1394155
Schmidt E, Shaligram A, Reynoso JF, Kothari V, Oleynikov D (2014) Hiatal hernia repair with biologic mesh reinforcement reduces recurrence rate in small hiatal hernias. Dis Esophagus 27:13–17. https://doi.org/10.1111/dote.12042
Ward KC, Costello KP, Baalman S, Pierce RA, Deeken CR, Frisella MM, Michael Brunt L, Matthews BD (2015) Effect of acellular human dermis buttress on laparoscopic hiatal hernia repair. Surg Endosc 29:2291–2297. https://doi.org/10.1007/s00464-014-3946-3
Pfluke JM, Parker M, Bowers SP, Asbun HJ, Daniel SC (2012) Use of mesh for hiatal hernia repair: a survey of SAGES members. Surg Endosc 26:1843–1848. https://doi.org/10.1007/s00464-009-0718-6
Asti E, Sironi A, Bonitta G, Lovece A, Milito P, Bonavina L (2017) Crura augmentation with Bio-A® mesh for laparoscopic repair of hiatal hernia: single-institution experience with 100 consecutive patients. Hernia 21(4):623–628. https://doi.org/10.1007/s10029-017-1603-1
Priego Jiménez P, Salvador Sanchís JL, Angel V, Escrig-Sos J (2014) Short-term results for laparoscopic repair of large paraesophageal hiatal hernias with Gore Bio A® mesh. Int J Surg 12(8):794–797. https://doi.org/10.1016/j.ijsu.2014.06.001
Massullo JM, Singh TP, Dunnican WJ, Binetti BR (2012) Preliminary study of hiatal hernia repair using polyglycolic acid: trimethylene carbonate mesh. JSLS 16(1):55–59. https://doi.org/10.4293/108680812X13291597715943
Korwar V, Adjepong S, Pattar J, Sigurdsson A (2019) Biological mesh repair of paraesophageal hernia: an analysis of our outcomes. J Laparoendosc Adv Surg Tech A 29(11):1446–1450. https://doi.org/10.1089/lap.2019.0423
Asti E, Lovece A, Bonavina L, Milito P, Sironi A, Bonitta G, Siboni S (2016) Laparoscopic management of large hiatus hernia: five-year cohort study and comparison of mesh-augmented versus standard crura repair. Surg Endosc 30(12):5404–5409. https://doi.org/10.1007/s00464-016-4897-7
Williams SF, Martin DP, Moses AC (2016) The history of GalaFLEX P4HB Scaffold. Aesthetic Surg J 36(suppl 2):S33–S42. https://doi.org/10.1093/asj/sjw141
Panici Tonucci T, Asti E, Sironi A, Ferrari D, Bonavina L (2020) Safety and efficacy of crura augmentation with phasix ST mesh for large hiatal hernia: 3-year single-center experience. J Laparoendosc Adv Surg Tech A 30(4):369–372. https://doi.org/10.1089/lap.2019.0726
Iossa A, Silecchia G (2019) Mid-term safety profile evaluation of Bio-A absorbable synthetic mesh as cruroplasty reinforcement. Surg Endosc 33(11):3783–3789. https://doi.org/10.1007/s00464-019-06676-3
Silecchia G, Iossa A, Cavallaro G, Rizzello M, Longo F (2014) Reinforcement of hiatal defect repair with absorbable mesh fixed with non-permanent devices. Minim Invasive Ther Allied Technol 23(5):302–308. https://doi.org/10.3109/13645706.2014.909853
Berselli M, Livraghi L, Latham L, Farassino L, Rota Bacchetta GL, Pasqua N, Ceriani I, Segato S, Cocozza E (2015) Laparoscopic repair of voluminous symptomatic hiatal hernia using absorbable synthetic mesh. Minim Invasive Ther Allied Technol 24(6):372–376. https://doi.org/10.3109/13645706.2015.1064446
Olson MT, Singhal S, Panchanathan R, Roy SB, Kang P, Ipsen T, Mittal SK, Huang JL, Smith MA, Bremner RM (2018) Primary paraesophageal hernia repair with Gore® Bio-A® tissue reinforcement: long-term outcomes and association of BMI and recurrence. Surg Endosc 32(11):4506–4516. https://doi.org/10.1007/s00464-018-6200-6
Gebhart A, Vu S, Armstrong C, Smith BR, Nguyen NT (2013) Initial outcomes of laparoscopic paraesophageal hiatal hernia repair with mesh. Am Surg 79(10):1017–1021. https://doi.org/10.1177/000313481307901013
Jones R, Simorov A, Lomelin D, Tadaki C, Oleynikov D (2015) Long-term outcomes of radiologic recurrence after paraesophageal hernia repair with mesh. Surg Endosc 29(2):425–430. https://doi.org/10.1007/s00464-014-3690-8
Gantert WA, Patti MG, Arcerito M, Feo C, Stewart L, DePinto M, Bhoyrul S, Rangel S, Tyrrell D, Fujino Y, Mulvihill SJ, Way LW (1998) Laparoscopic repair of paraesophageal hiatal hernias. J Am Coll Surg 186(4):428–432. https://doi.org/10.1016/s1072-7515(98)00061-1
Mattar SG, Bowers SP, Galloway KD, Hunter JG, Smith CD (2002) Long-term outcome of laparoscopic repair of paraesophageal hernia. Surg Endosc 16(5):745–749. https://doi.org/10.1007/s00464-001-8194-7
Wiechmann RJ, Ferguson MK, Naunheim KS, McKesey P, Hazelrigg SJ, Santucci TS, Macherey RS, Landreneau RJ (2001) Laparoscopic management of giant paraesophageal herniation. Ann Thorac Surg 71(4):1080–1086. https://doi.org/10.1016/s0003-4975(00)01229-7 (discussion 1086-7)
Furnée EJ, Draaisma WA, Simmermacher RK, Stapper G, Broeders IA (2010) Long-term symptomatic outcome and radiologic assessment of laparoscopic hiatal hernia repair. Am J Surg 199(5):695–701. https://doi.org/10.1016/j.amjsurg.2009.03.008
Poncet G, Robert M, Roman S, Boulez JC (2010) Laparoscopic repair of large hiatal hernia without prosthetic reinforcement: late results and relevance of anterior gastropexy. J Gastrointest Surg 14(12):1910–1916. https://doi.org/10.1007/s11605-010-1308-6
Daigle CR, Funch-Jensen P, Calatayud D, Rask P, Jacobsen B, Grantcharov TP (2015) Laparoscopic repair of paraesophageal hernia with anterior gastropexy: a multicenter study. Surg Endosc 29(7):1856–1861. https://doi.org/10.1007/s00464-014-3877-z
Oor JE, Roks DJ, Koetje JH, Broeders JA, van Westreenen HL, Nieuwenhuijs VB, Hazebroek EJ (2018) Randomized clinical trial comparing laparoscopic hiatal hernia repair using sutures versus sutures reinforced with non-absorbable mesh. Surg Endosc 32(11):4579–4589. https://doi.org/10.1007/s00464-018-6211-3
Ilyashenko VV, Grubnyk VV, Grubnik VV (2018) Laparoscopic management of large hiatal hernia: mesh method with the use of ProGrip mesh versus standard crural repair. Surg Endosc 32(8):3592–3598. https://doi.org/10.1007/s00464-018-6087-2
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Benjamin Clapp, Ali M. Kara, John D. Marr, Paul J Nguyen-Lee, Hani M Annabi, Luis Alvarado; Omar M Ghanem and Brian Davis have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clapp, B., Kara, A.M., Nguyen-Lee, P.J. et al. Does bioabsorbable mesh reduce hiatal hernia recurrence rates? A meta-analysis. Surg Endosc 37, 2295–2303 (2023). https://doi.org/10.1007/s00464-022-09514-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09514-1