Abstract
Introduction
A high proportion of colorectal surgery patients within an enhanced recovery pathway (ERP) do not experience complications but remain hospitalized mainly waiting for gastrointestinal (GI) recovery. Accurate identification of these patients may allow discharge prior to the return of GI function. Therefore, the objective of this study is to determine if tolerating clear fluid (CF) on postoperative day (POD) 0 was associated with uncomplicated return of GI function after laparoscopic colorectal surgery.
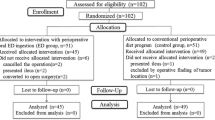
Methods
Pooled data from three prospective studies from a single specialist colorectal referral center were analyzed (2013–2019). The present study included adult patients that underwent elective laparoscopic colectomy without stoma. Postoperative GI symptoms were collected daily in all three datasets. The main exposure variable, whether CF diet was tolerated on POD0, was defined as patients drinking at least 300 mL of CF without any nausea, anti-emetics, or vomiting (CF+ vs CF−). The main outcome measure was time to GI-3 (tolerating solid diet and passage of gas or stools).
Results
A total of 221 patients were included in this study, including 69% CF+ and 31% CF−. The groups were similar in age, gender, and comorbidities, but the CF− patients were more likely to have surgery for inflammatory bowel disease. CF+ patients had faster time to GI-3 (mean 1.6d (SD 0.7) vs. 2.3d (SD 1.5), p < 0.001). The CF+ group also experienced fewer complications (19% vs. 35%, p = 0.009), shorter mean LOS (mean 3.6d (SD 2.9) vs. 6.2d (SD 9.4), p = 0.002), and were more likely to be discharged by the target LOS (66% vs. 50%, p = 0.024).
Conclusion
Toleration of CF on POD0 was associated with faster return of GI function, fewer complications, and shorter LOS. This may be used as a criteria for potential discharge prior to full return of GI function after laparoscopic colectomy within an ERP.
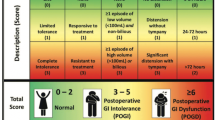
Graphical abstract


Adapted from Hedrick et al. [16]

Similar content being viewed by others
References
Alhashemi M, Fiore JF Jr, Safa N, Al Mahroos M, Mata J, Pecorelli N, Baldini G, Dendukuri N, Stein BL, Liberman AS, Charlebois P, Carli F, Feldman LS (2019) Incidence and predictors of prolonged postoperative ileus after colorectal surgery in the context of an enhanced recovery pathway. Surg Endosc 33:2313–2322
Delaney CP (2008) Outcome of discharge within 24 to 72 hours after laparoscopic colorectal surgery. Dis Colon Rectum 51:181–185
Gignoux B, Gosgnach M, Lanz T, Vulliez A, Blanchet MC, Frering V, Faucheron JL, Chasserant P (2019) Short-term outcomes of ambulatory colectomy for 157 consecutive patients. Ann Surg 270:317–321
Mata J, Pecorelli N, Kaneva P, Moldoveanu D, Gosselin-Tardiff A, Alhashemi M, Robitaille S, Balvardi S, Lee L, Stein BL, Liberman S, Charlebois P, Fiore JF Jr, Feldman LS (2020) A mobile device application (app) to improve adherence to an enhanced recovery program for colorectal surgery: a randomized controlled trial. Surg Endosc 34:742–751
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z (2013) Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum 56:667–678
Fiore JF Jr, Browning L, Bialocerkowski A, Gruen RL, Faragher IG, Denehy L (2012) Hospital discharge criteria following colorectal surgery: a systematic review. Colorectal Dis 14:270–281
Fiore JF Jr, Bialocerkowski A, Browning L, Faragher IG, Denehy L (2012) Criteria to determine readiness for hospital discharge following colorectal surgery: an international consensus using the Delphi technique. Dis Colon Rectum 55:416–423
Vather R, Bissett I (2013) Management of prolonged post-operative ileus: evidence-based recommendations. ANZ J Surg 83:319–324
Munk-Madsen P, Eriksen JR, Kehlet H, Gogenur I (2019) Why still in hospital after laparoscopic colorectal surgery within an enhanced recovery programme? Colorectal Dis 21:1438–1444
Bednarski BK, Nickerson TP, You YN, Messick CA, Speer B, Gottumukkala V, Manandhar M, Weldon M, Dean EM, Qiao W, Wang X, Chang GJ (2019) Randomized clinical trial of accelerated enhanced recovery after minimally invasive colorectal cancer surgery (RecoverMI trial). Br J Surg 106:1311–1318
EuroSurg C (2020) Safety of hospital discharge before return of bowel function after elective colorectal surgery. Br J Surg 107:552–559
Gomez-Izquierdo JC, Trainito A, Mirzakandov D, Stein BL, Liberman S, Charlebois P, Pecorelli N, Feldman LS, Carli F, Baldini G (2017) Goal-directed fluid therapy does not reduce primary postoperative ileus after elective laparoscopic colorectal surgery: a randomized controlled trial. Anesthesiology 127:36–49
Fiore JF Jr, Castelino T, Pecorelli N, Niculiseanu P, Balvardi S, Hershorn O, Liberman S, Charlebois P, Stein B, Carli F, Mayo NE, Feldman LS (2017) Ensuring early mobilization within an enhanced recovery program for colorectal surgery: a randomized controlled trial. Ann Surg 266:223–231
Vaughan-Shaw PG, Fecher IC, Harris S, Knight JS (2012) A meta-analysis of the effectiveness of the opioid receptor antagonist alvimopan in reducing hospital length of stay and time to GI recovery in patients enrolled in a standardized accelerated recovery program after abdominal surgery. Dis Colon Rectum 55:611–620
Wolthuis AM, Bislenghi G, Fieuws S, de Buck van Overstraeten A, Boeckxstaens G, D’Hoore A (2016) Incidence of prolonged postoperative ileus after colorectal surgery: a systematic review and meta-analysis. Colorectal Dis 18:O1-9
Hedrick TL, McEvoy MD, Mythen MMG, Bergamaschi R, Gupta R, Holubar SD, Senagore AJ, Gan TJ, Shaw AD, Thacker JKM, Miller TE, Wischmeyer PE, Carli F, Evans DC, Guilbert S, Kozar R, Pryor A, Thiele RH, Everett S, Grocott M, Abola RE, Bennett-Guerrero E, Kent ML, Feldman LS, Fiore JF Jr, Perioperative Quality Initiative W (2018) American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on postoperative gastrointestinal dysfunction within an enhanced recovery pathway for elective colorectal surgery. Anesth Analg 126:1896–1907
Jamal MH, Karam A, Alsharqawi N, Buhamra A, AlBader I, Al-Abbad J, Dashti M, Abulhasan YB, Almahmeed H, AlSabah S (2019) Laparoscopy in acute care surgery: repair of perforated duodenal ulcer. Med Princ Pract 28:442–448
Leung V, Alsharqawi N, Baldini G, Liberman AS, Charlebois P, Stein B, Fiore JF Jr, Feldman LS, Lee L (2021) Trajectory of gastrointestinal function after laparoscopic colorectal surgery within an enhanced recovery pathway. Annual Meeting of the Central Surgical Association, Chicago
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Mata J, Fiore JF Jr, Pecorelli N, Stein BL, Liberman S, Charlebois P, Feldman LS (2018) Predictors of adherence to enhanced recovery pathway elements after laparoscopic colorectal surgery. Surg Endosc 32:1812–1819
Dai X, Ge X, Yang J, Zhang T, Xie T, Gao W, Gong J, Zhu W (2017) Increased incidence of prolonged ileus after colectomy for inflammatory bowel diseases under ERAS protocol: a cohort analysis. J Surg Res 212:86–93
Lee L, Tran T, Mayo NE, Carli F, Feldman LS (2014) What does it really mean to “recover” from an operation? Surgery 155:211–216
Mann-Farrar J, Egan E, Higgins A, Wysocki L, Vaux A, Arndell E, Burmeister EA (2019) Are postoperative clinical outcomes influenced by length of stay in the postanesthesia care unit? J Perianesth Nurs 34:386–393
Lee L, Eustache J, Baldini G, Liberman AS, Charlebois P, Stein B, Fiore JFF, Jr., Feldman LS (2021) Enhanced recovery 2.0—same day discharge with mobile app follow-up after minimally invasive colorectal surgery. Ann Surg (in press)
Slim K, Reymond T, Joris J, Paul S, Pereira B, Cotte E (2020) Intolerance to early oral feeding in enhanced recovery after colorectal surgery: an early red flag? Colorectal Dis 22:95–101
Trepanier M, Valin-Thorburn A, Kouyoumdjian A, Dumitra T, Alhashemi M, Kaneva P, Liberman AS, Charlebois P, Stein BS, Fried GM, Feldman LS, Lee L (2019) Intracorporeal versus extracorporeal anastomosis for right colectomy does not affect gastrointestinal recovery within an enhanced recovery after surgery program. Surg Endosc
Pecorelli N, Hershorn O, Baldini G, Fiore JF Jr, Stein BL, Liberman AS, Charlebois P, Carli F, Feldman LS (2017) Impact of adherence to care pathway interventions on recovery following bowel resection within an established enhanced recovery program. Surg Endosc 31:1760–1771
Funding
LL is supported by a Career Development Award (CDA-019) from the American Society of Colon and Rectal Surgeons Research Foundation. This study was in part funded by the 2020 CSA Foundation Turcotte Award from the Central Surgical Association.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Lee is the recipient of an investigator-initiated research grant from Johnson & Johnson Canada and is also supported by a Career Development Award from the American Society of Colon and Rectal Surgeons (CDA-019). This study was in part funded by the 2020 CSA Foundation Turcotte Award from the Central Surgical Association. Drs. Leung, Baldini, Liberman, Charlebois, Stein, Feldman, and Fiore Jr. have no conflicts of interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leung, V.W.Y., Baldini, G., Liberman, S. et al. Tolerating clear fluids diet on postoperative day 0 predicts early recovery of gastrointestinal function after laparoscopic colectomy. Surg Endosc 36, 9262–9272 (2022). https://doi.org/10.1007/s00464-022-09151-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09151-8