Abstract
Background
The objective of this study is to assess surgical outcomes following the initial use of laparoscopy versus laparotomy when managing patients with hollow viscus injuries due to trauma.
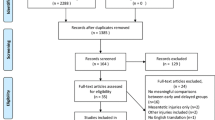
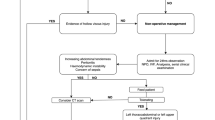
Methods
Using the database from the American College of Surgeons Trauma Quality Improvement Program we identified all patients from 2015–2017 with ICD-10 Diagnosis codes for hollow viscus trauma. Types of procedures were identified by ICD-10 PCS codes. Patient outcomes were stratified by major trauma(ISS > 15) and minor trauma. Continuous variables were compared by ANOVA and categorical variables compared by Chi-Square. Analysis performed using STATA 16.
Results
We identified 16,284 patients that matched inclusion criteria within the study time frame. Of those, 1986 patients received a surgical intervention, 1911(96%) were open and 75(4%) were laparoscopic. In blunt trauma there were 106 diagnostic procedures, 87(82%) were open and 19(18%) were laparoscopic. There were 574 therapeutic procedures, 543(95%) were open and 31(5%) were laparoscopic. In penetrating trauma there were 223 diagnostic procedures, 215(96%) were open and 8(4%) were laparoscopic. There were 1039 therapeutic procedures for penetrating trauma, 1023(98%) were open and 16(2%) were laparoscopic. For minor trauma, mean length of stay(days) after open surgery was 5 while for laparoscopy it was 2 (p = 0.04). There were 203 complications noted in the open group and 7 in the laparoscopic group (p = 0.19). For major trauma, mean length of stay(days) after open surgery was 5 and 6 for laparoscopy p = 0.54). There were 242 complications in the open group and 1 in the laparoscopic group (p = 0.07). There was no noted significant difference noted in the disposition at discharge in either group in both major and minor trauma.
Conclusions
For those that required surgery for hollow viscous injury, laparoscopy appeared to be safe, had less adverse outcomes and was underutilized, particularly when only a diagnostic procedure was required.
Similar content being viewed by others
References
Watts DD, Fakhry SM (2003) EAST Multi-Institutional Hollow Viscus Injury Research Group Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. J Trauma 54(2):289–294. https://doi.org/10.1097/01.TA.0000046261.06976.6A
Williams MD, Watts D, Fakhry S (2003) Colon injury after blunt abdominal trauma: results of the EAST Multi-Institutional Hollow Viscus Injury Study. J Trauma 55(5):906–912. https://doi.org/10.1097/01.TA.0000093243.01377.9B
Bonomi AM, Granieri S, Gupta S, Altomare M, Cioffi SPB, Sammartano F, Cimbanassi S, Chiara O (2021) Traumatic hollow viscus and mesenteric injury: role of CT and potential diagnostic-therapeutic algorithm. Updates Surg. 73(2):703–710. https://doi.org/10.1007/s13304-020-00929-w
Bège T, Brunet C, Berdah SV (2016) Hollow viscus injury due to blunt trauma: A review. J Visc Surg 153(4 Suppl):61–68. https://doi.org/10.1016/j.jviscsurg.2016.04.007
Achatz G, Schwabe K, Brill S, Zischek C, Schmidt R, Friemert B, Beltzer C (2020) Diagnostic options for blunt abdominal trauma. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-020-01405-1
LeBedis CA, Anderson SW, Bates DD, Khalil R, Matherly D, Wing H, Burke PA, Soto JA (2016) CT imaging signs of surgically proven bowel trauma. Emerg Radiol 23(3):213–219. https://doi.org/10.1007/s10140-016-1380-7
Khubutiya MSh, Yartsev PA, Guliaev AA, Levitsky VD, Tlibekova MA (2013) Laparoscopy in blunt and penetrating abdominal trauma. Surg Laparosc Endosc Percutan Tech 23(6):507–512. https://doi.org/10.1097/SLE.0b013e3182937c37
Gao Y, Li S, Xi H, Bian S, Zhang K, Cui J, Li J, Liu F, Liu Y, Lu Y, Wang B, Qiao Z, Chen L (2020) Laparoscopy versus conventional laparotomy in the management of abdominal trauma: a multi-institutional matched-pair study. Surg Endosc 34(5):2237–2242. https://doi.org/10.1007/s00464-019-07013-4
Kaban GK, Novitsky YW, Perugini RA, Haveran L, Czerniach D, Kelly JJ, Litwin DE (2008) Use of laparoscopy in evaluation and treatment of penetrating and blunt abdominal injuries. Surg Innov 15(1):26–31. https://doi.org/10.1177/1553350608314664
Trejo-Ávila ME, Valenzuela-Salazar C, Betancourt-Ferreyra J, Fernández-Enríquez E, Romero-Loera S, Moreno-Portillo M (2017) Laparoscopic versus open surgery for abdominal trauma: A case-matched study. J Laparoendosc Adv Surg Tech A 27(4):383–387. https://doi.org/10.1089/lap.2016.0535
Coccolini F, Catena F, Pisano M, Gheza F, Fagiuoli S, Di Saverio S, Leandro G, Montori G, Ceresoli M, Corbella D, Sartelli M, Sugrue M, Ansaloni L (2015) Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. 18:196–204. PMID: 25958296 https://doi.org/10.1016/j.ijsu.2015.04.083
Liu Y, Cui Z, Zhang R (2017) Laparoscopic Versus Open Appendectomy for Acute Appendicitis in Children. Indian Pediatr 54(11):938–941. https://doi.org/10.1007/s13312-017-1186-z
Funding
This research did not receive any specific grant or funding from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Andrew Litwin, John Romanelli, and Michael Tirabassi and Ms. Aixa Perez Coulter have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Litwin, A., Coulter, A.P., Romanelli, J. et al. Use of minimally invasive surgery for the management of hollow viscus traumatic injuries. Surg Endosc 36, 8421–8429 (2022). https://doi.org/10.1007/s00464-022-09102-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09102-3