Abstract
Background
Duodenal subepithelial lesions (D-SELs) are rare and their resection is challenging. Unfortunately, data on surgical and endoscopic resection of D-SELs are scarce. This study aimed to assess the safety and efficacy of surgical resection and endoscopic resection (ER) for D-SELs.
Methods
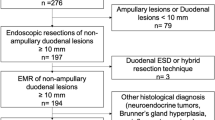
We retrospectively analyzed clinical data of patients with non-ampullary D-SELs who underwent ER or surgery and compared the outcomes between ER and surgery with no/low-risk SELs over 15 mm from March 2010 to August 2020. Clinicopathologic findings, procedure-related parameters, and follow-up data were analyzed.
Results
A total of 107 patients (108 lesions) were enrolled; 52 patients (53 lesions) received ER and 55 patients (55 lesions) received surgery. In ER group, en bloc resection rate and R0 resection rate were 94 and 89%, respectively. Major adverse events rate was 6%. One (2%) patient experienced local recurrence. In surgery group, R0 resection was achieved in all cases. Major adverse events rate was 20%. Recurrence rate and distant metastases rate were 4 and 8%, respectively. One (2%) patient died from septicemia during follow-up. Thirty-three patients in each group were enrolled in the comparison. There were no significant differences in age, sex, lesion size and location (P > 0.05). More histologically GISTs and muscularis propria-originated lesions were treated by surgery (P < 0.05). ER was significantly associated with a shorter operation time, shorter hospital stay, lower cost, less estimated blood loss, and lower major adverse events rate compared to the surgery group (P < 0.05). However, R0 resection rate, mortality, recurrence rate, and metastases rate were not significant different (P > 0.05).
Conclusions
ER is an effective and safe treatment modality for selected patients with non-ampullary D-SELs by expert endoscopists. Surgery is a radical method for D-SELs that should be reserved for D-SELs not amenable to ER.


Similar content being viewed by others
References
Cho JW, Korean ESD Study Group (2016) Current guidelines in the management of upper gastrointestinal subepithelial tumors. Clinical endoscopy 49:235–240
Reddymasu SC, Oropeza-Vail M, Pakseresht K et al (2012) Are endoscopic ultrasonography imaging characteristics reliable for the diagnosis of small upper gastrointestinal subepithelial lesions? J Clin Gastroenterol 46:42–45
Gaspar JP, Stelow EB, Wang AY (2016) Approach to the endoscopic resection of duodenal lesions. World J Gastroenterol 22:600–617
Delle Fave G, O’Toole D, Sundin A et al (2016) ENETS consensus guidelines update for gastroduodenal neuroendocrine neoplasms. Neuroendocrinology 103:119–124
Shamali A, McCrudden R, Bhandari P et al (2016) Pancreaticoduodenectomy for nonampullary duodenal lesions: indications and results. Eur J Gastroenterol Hepatol 28:1388–1393
Lu C, Jin W, Mou Y et al (2020) Optimal laparoscopic management and oncological outcomes of gastrointestinal stromal tumors in duodenum: pancreaticoduodenectomy or pancreas-sparing duodenectomy? Cancer Manag Res 12:4725–4734
Dasari BVM, Al-Shakhshir S, Pawlik TM et al (2018) Outcomes of surgical and endoscopic resection of duodenal neuroendocrine tumours (NETs): a systematic review of the literature. J Gastrointest Surg 22:1652–1658
Zhou Y, Wang X, Si X et al (2020) Surgery for duodenal gastrointestinal stromal tumor: a systematic review and meta-analysis of pancreaticoduodenectomy versus local resection. Asian J Surg 43:1–8
Du H, Ning L, Li S et al (2020) Diagnosis and treatment of duodenal gastrointestinal stromal tumors. Clin Transl Gastroenterol 11:e00156
Cameron JL, Riall TS, Coleman J et al (2006) One thousand consecutive pancreaticoduodenectomies. Ann Surg 244:10–15
Shen Z, Chen P, Du N et al (2019) Pancreaticoduodenectomy versus limited resection for duodenal gastrointestinal stromal tumors: a systematic review and meta-analysis. BMC Surg 19:121
Bartel MJ, Puri R, Brahmbhatt B et al (2018) Endoscopic and surgical management of nonampullary duodenal neoplasms. Surg Endosc 32:2859–2869
Kim TW, Kim GH, Park DY et al (2017) Endoscopic resection for duodenal subepithelial tumors: a single-center experience. Surg Endosc 31:1936–1946
Ye LP, Mao XL, Zheng HH et al (2017) Safety of endoscopic resection for duodenal subepithelial lesions with wound closure using clips and an endoloop: an analysis of 68 cases. Surg Endosc 31:1070–1077
Lee SW, Sung JK, Cho YS et al (2019) Comparisons of therapeutic outcomes in patients with nonampullary duodenal neuroendocrine tumors (NADNETs): a multicenter retrospective study. Medicine 98:e16154–e16154
Ren Z, Lin S-L, Zhou P-H et al (2019) Endoscopic full-thickness resection (EFTR) without laparoscopic assistance for nonampullary duodenal subepithelial lesions: our clinical experience of 32 cases. Surg Endosc 33:3605–3611
Gincul R, Ponchon T, Napoleon B et al (2016) Endoscopic treatment of sporadic small duodenal and ampullary neuroendocrine tumors. Endoscopy 48:979–986
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Tan Y, Tang X, Guo T et al (2017) Comparison between submucosal tunneling endoscopic resection and endoscopic full-thickness resection for gastric stromal tumors originating from the muscularis propria layer. Surg Endosc 31:3376–3382
Chok A-Y, Koh Y-X, Ow MYL et al (2014) A systematic review and meta-analysis comparing pancreaticoduodenectomy versus limited resection for duodenal gastrointestinal stromal tumors. Ann Surg Oncol 21:3429–3438
Joensuu H (2008) Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Hum Pathol 39:1411–1419
Li C, Chu Y, Lv L et al (2021) Safety and efficacy of endoscopic resection for the treatment of duodenal subepithelial lesions. J Gastrointest Oncol 12:856–863
Zhang H, Liu Q (2020) Prognostic indicators for gastrointestinal stromal tumors: a review. Trans Oncol 13:100812
Zhong Y, Deng M, Liu B et al (2013) Primary gastrointestinal stromal tumors: current advances in diagnostic biomarkers, prognostic factors and management of its duodenal location. Intractable Rare Dis Res 2:11–17
Liu Z, Zheng G, Liu J et al (2018) Clinicopathological features, surgical strategy and prognosis of duodenal gastrointestinal stromal tumors: a series of 300 patients. BMC Cancer 18:563
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: CL, DL, and YT, (II) Analysis and interpretation of the data: CL, CL, XW, and ML, (III) Drafting of the article: CL and YT, (IV) Critical revision of the article for important intellectual content: CL, DL, and YT, (V) Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Disclosures
Drs. Chen Li, Chengbai Liang, Xuehong Wang, Meixian Le, Deliang Liu, and Yuyong Tan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, C., Liang, C., Wang, X. et al. Safety and efficacy of surgical and endoscopic resection in the treatment of duodenal subepithelial lesions. Surg Endosc 36, 4145–4153 (2022). https://doi.org/10.1007/s00464-021-08740-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08740-3