Abstract
Background
Surgical resection is a mainstay of treatment for colorectal cancer (CRC). Minimally invasive surgery (MIS) has been shown to have improved outcomes compared to open procedures for colorectal malignancy. While use of MIS has been increasing, there remains large variability in its implementation at the hospital and patient level.
Objective
The purpose of this study was to identify disparities in sex, race, location, patient income status, insurance status, hospital region, bed size and teaching status for the use of MIS in the treatment of CRC.
Methods
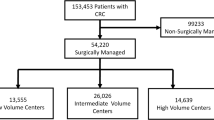
This was a retrospective cohort study using the Nationwide Inpatient Sample Database. Between 2008 and 2017, there were 412,292 hospitalizations of adult patients undergoing elective colectomy for CRC. The primary outcome was use of MIS during hospitalization.
Results
Overall, the frequency of open colectomies was higher than MIS (56.56% vs. 43.44%). Black patients were associated with decreased odds of MIS use during hospitalization compared to White patients (OR 0.921, p = 0.0011). As the county population where patients resided decreased, odds of MIS also significantly decreased as compared to central counties of metropolitan areas. As income decreased below the reference of $71,000, odds of MIS also significantly decreased. Medicaid and uninsured patients had decreased odds of MIS use during hospitalization compared to private insurance (OR 0.751, p < 0.0001 and OR 0.629, p < 0.0001 respectively). Rural and urban non-teaching hospitals were associated with decreased odds of MIS as compared to urban teaching hospitals (OR 0.523, p < 0.0001 and OR 0.837, p < 0.0001 respectively). Hospitals with a small bed size were also associated with decreased MIS during hospitalizations (OR 0.888, p < 0.0001).
Conclusions
Marked hospital level and socioeconomic disparities exist for utilization of MIS for colorectal cancer. Strategies targeted at reducing these gaps have the potential to improve surgical outcomes and cancer survival.

Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62(1):10–29
McCombie AM, Frizelle BPF et al (2018) The ALCCaS trial: a randomized controlled trial comparing quality of life following laparoscopic versus open colectomy for colon cancer. Dis Colon Rectum 61(10):1156–1162
Deijen CL, Vasmel JE, de Lange-de Klerk ESM et al (2017) Ten-year outcomes of a randomised trial of laparoscopic versus open surgery for colon cancer. Surg Endosc 31(6):2607–2615
Kitano S, Inomata M, Mizusawa J et al (2017) Survival outcomes following laparoscopic versus open D3 dissection for stage II or III colon cancer (JCOG0404): a phase 3, randomised controlled trial. Lancet Gastroenterol Hepatol 2(4):261–268
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Guillou PJ, Quirke P, Thorpe H et al (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Cirocchi R, Cesare Campanile F, Di Saverio S et al (2017) Laparoscopic versus open colectomy for obstructing right colon cancer: A systematic review and meta-analysis. J Visc Surg 154(6):387–399
Nelson H, Sargent DJ, Wieand HJ et al (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Noblett SE, Horgan AF (2007) A prospective case-matched comparison of clinical and financial outcomes of open versus laparoscopic colorectal resection. Surg Endosc 21(3):404–408
Wei D, Johnston S, Goldstein L, Nagle D (2020) Minimally invasive colectomy is associated with reduced risk of anastomotic leak and other major perioperative complications and reduced hospital resource utilization as compared with open surgery: a retrospective population-based study of comparative effectiveness and trends of surgical approach. Surg Endosc 34(2):610–621
Xu T, Hutfless SM, Cooper MA, Zhou M, Massie AB, Makary MA (2015) Hospital cost implications of increased use of minimally invasive surgery. JAMA Surg 150(5):489–490
Xu T, Makary MA, Al Kazzi E, Zhou M, Pawlik TM, Hutfless SM (2016) Surgeon-level variation in postoperative complications. J Gastrointest Surg 20(7):1393–1399
Cooper MA, Hutfless S, Segev DL, Brahim A, Yu H, Makary MA (2014) Hospital level under-utilization of minimally invasive surgery in the United States: retrospective review. Bmj. 349:g4198
Alnasser M, Schneider EB, Gearhart SL et al (2014) National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc 28(1):49–57
Moghadamyeghaneh Z, Carmichael JC, Mills S, Pigazzi A, Nguyen NT, Stamos MJ (2015) Variations in laparoscopic colectomy utilization in the United States. Dis Colon Rectum 58(10):950–956
Breen N, Lewis DR, Gibson JT, Yu M, Harper J (2017) Assessing disparities in colorectal cancer mortality by socioeconomic status using new tools: health disparities calculator and socioeconomic quintiles. Cancer Causes Control 28(2):117–125
(HCUP), 2019 H.C.a.U.P. HCUP databases. Available from: www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 3 May 2020
Khera R, Angraal S, Couch T et al (2017) Adherence to methodological standards in research using the national inpatient sample. JAMA 318(20):2011–2018
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1):8–27
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ (2009) A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care 47(6):626–633
Thompson NR, Fan Y, Dalton JE et al (2015) A new Elixhauser-based comorbidity summary measure to predict in-hospital mortality. Med Care 53(4):374–379
Hawkins AT, Ford MM, Benjamin Hopkins M et al (2018) Barriers to laparoscopic colon resection for cancer: a national analysis. Surg Endosc 32(2):1035–1042
Wu Q, Wei M, Ye Z et al (2017) Laparoscopic colectomy versus open colectomy for treatment of transverse colon cancer: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A 27(10):1038–1050
Hayashi H, Ozaki N, Ogawa K et al (2018) Assessing the economic advantage of laparoscopic vs. open approaches for colorectal cancer by a propensity score matching analysis. Surg Today 48(4):439–448
Kim RH, Kavanaugh MM, Caldito GC (2017) Laparoscopic colectomy for cancer: Improved compliance with guidelines for chemotherapy and survival. Surgery 161(6):1633–1641
Czaykowski PM, Gill S, Kennecke HF, Gordon VL, Turner D (2011) Adjuvant chemotherapy for stage III colon cancer: does timing matter? Dis Colon Rectum 54(9):1082–1089
Berglund A, Cedermark B, Glimelius B (2008) Is it deleterious to delay the start of adjuvant chemotherapy in colon cancer stage III? Ann Oncol 19(2):400–402
Park A, Kavic SM, Lee TH, Heniford BT (2007) Minimally invasive surgery: the evolution of fellowship. Surgery 142(4):505–511 (discussion 511–3)
Rattner DW, Apelgren KN, Eubanks WS (2001) The need for training opportunities in advanced laparoscopic surgery. Surg Endosc 15(10):1066–1070
Freischlag K, Adam M, Turner M et al (2019) With widespread adoption of MIS colectomy for colon cancer, does hospital type matter? Surg Endosc 33(1):159–168
Sheetz KH, Clafin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911
Robinson CN, Balentine CJ, Sansgiry S, Berger DH (2012) Disparities in the use of minimally invasive surgery for colorectal disease. J Gastrointest Surg. 16(5):897–903 (discussion 903–4)
Singla A, Simons JP, Carroll JE et al (2010) Hospital volume as a surrogate for laparoscopically assisted colectomy. Surg Endosc 24(3):662–669
Vu JV, Gunaseelan V, Krapohl GL, Englesbe MJ, Campbell DA Jr, Dimick JB, Telem DA (2019) Surgeon utilization of minimally invasive techniques for inguinal hernia repair: a population-based study. Surg Endosc 33(2):486–493
Mehta A, Xu T, Hutfless S, Makary MA, Sinno AK, Tanner EJ, Stone RL, Wang K, Fader AN (2017) Patient, surgeon, and hospital disparities associated with benign hysterectomy approach and perioperative complications. Am J Obstet Gynecol 216(5):497.e1-497.e10
Zheng Z, Jemal A, Lin CC, Hu CY, Chang GJ (2015) Comparative effectiveness of laparoscopy vs open colectomy among nonmetastatic colon cancer patients: an analysis using the National Cancer Data Base. J Natl Cancer Instit 107(3):91
Akinyemiju T, Meng Q, Vin-Raviv N (2016) Race/ethnicity and socio-economic differences in colorectal cancer surgery outcomes: analysis of the nationwide inpatient sample. BMC Cancer 16(1):715
Ratnapradipa KL, Lian M, Jeffe DB et al (2017) Patient, hospital, and geographic disparities in laparoscopic surgery use among surveillance, epidemiology, and end results-medicare patients with colon cancer. Dis Colon Rectum 60(9):905–913
Mainor AJ, Morden NE, Smith J, Tomlin S, Skinner J (2019) ICD-10 Coding will challenge researchers: caution and collaboration may reduce measurement error and improve comparability over time. Med Care 57(7):e42–e46
Lau DT, Strashny A, Phan K, Blum AL, Burke-Bebee S (2018) Evaluation of Transition From ICD-9-CM to ICD-10-CM Diagnosis Coding System in the National Ambulatory Medical Care Survey. Natl Health Stat Rep 120:1–10
Funding
None.
Author information
Authors and Affiliations
Contributions
RP: Data collection, analysis and interpretation of data, manuscript drafting and editing, final approval of the version to be published. KP: Analysis and interpretation of data, manuscript drafting and editing, final approval of the version to be published. AM: Concept and design, critical manuscript revision, project supervision, final approval of the version to be published. MAD: Concept and design, critical manuscript revision, project supervision, final approval of the version to be published.
Corresponding author
Ethics declarations
Disclosures
Richa Patel, Krittika Pant, Krishan S. Patel, Aziz M. Merchant, and Melissa M. Alvarez-Downing have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Patel, R., Pant, K., Patel, K.S. et al. Association of hospital factors and socioeconomic status with the utilization of minimally invasive surgery for colorectal cancer over a decade. Surg Endosc 36, 3750–3762 (2022). https://doi.org/10.1007/s00464-021-08690-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08690-w