Abstract
Background
There is controversy regarding the widespread uptake of robotic surgery across several surgical disciplines. While it has been shown to confer clinical benefits such as decreased blood loss and shorter hospital stays, some argue that the benefits of this technology do not outweigh its high cost. We performed a retrospective insurance-based analysis to investigate how undergoing robotic surgery, compared to open surgery, may impact the time in which an employed individual returns to work after undergoing major surgery.
Methods
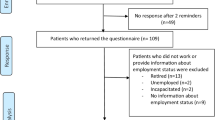
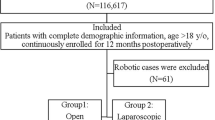
We identified a cohort of US adults with employer-sponsored insurance using claims data from the MarketScan database who underwent either open or robotic radical prostatectomy, hysterectomy/myomectomy, and partial colectomy from 2012 to 2016. We performed multiple regression models incorporating propensity scores to assess the effect of robotic vs. open surgery on the number of absent days from work, adjusting for demographic characteristics and baseline absenteeism.
Results
In a cohort of 1157 individuals with employer-sponsored insurance, those undergoing open surgery, compared to robotic surgery, had 9.9 more absent workdays for radical prostatectomy (95%CI 5.0 to 14.7, p < 0.001), 25.3 for hysterectomy/myomectomy (95%CI 11.0–39.6, p < 0.001), and 29.8 for partial colectomy (95%CI 14.8–44.8, p < 0.001)
Conclusion
For the three major procedures studied, robotic surgery was associated with fewer missed days from work compared to open surgery. This information helps payers, patients, and providers better understand some of the indirect benefits of robotic surgery relative to its cost.
Similar content being viewed by others
References
Sugerman DT (2013) JAMA patient page. Robotic surgery. JAMA 310:1086
Gandaglia G, Sammon JD, Chang SL et al (2014) Comparative effectiveness of robot-assisted and open radical prostatectomy in the postdissemination era. J Clin Oncol 32:1419–1426
Kim CW, Kim CH, Baik SH (2014) Outcomes of robotic-assisted colorectal surgery compared with laparoscopic and open surgery: a systematic review. J Gastrointest Surg 18:816–830
Martino MA, Berger EA, McFetridge JT et al (2014) A comparison of quality outcome measures in patients having a hysterectomy for benign disease: robotic vs. non-robotic approaches. J. Minimally Invas Gynecol 21:389–393
Moghadamyeghaneh Z, Hanna MH, Carmichael JC, Pigazzi A, Stamos MJ, Mills S (2016) Comparison of open, laparoscopic, and robotic approaches for total abdominal colectomy. Surg Endosc 30:2792–2798
Shah CA, Beck T, Liao JB, Giannakopoulos NV, Veljovich D, Paley P (2017) Surgical and oncologic outcomes after robotic radical hysterectomy as compared to open radical hysterectomy in the treatment of early cervical cancer. J Gynecol Oncol 28:e82
Trinh QD, Sammon J, Sun M et al (2012) Perioperative outcomes of robot-assisted radical prostatectomy compared with open radical prostatectomy: results from the nationwide inpatient sample. Eur Urol 61:679–685
Mottrie A, Larcher A, Patel V (2018) The past, the present, and the future of robotic urology: robot-assisted surgery and human-assisted robots. Eur Urol Focus 4:629–631
Berlinger NT (2006) Robotic surgery–squeezing into tight places. N Engl J Med 354:2099–2101
Aggarwal A, Lewis D, Mason M, Purushotham A, Sullivan R, van der Meulen J (2017) Effect of patient choice and hospital competition on service configuration and technology adoption within cancer surgery: a national, population-based study. Lancet Oncol 18:1445
Mirkin JN, Lowrance WT, Feifer AH, Mulhall JP, Eastham JE, Elkin EB (2012) Direct-to-consumer Internet promotion of robotic prostatectomy exhibits varying quality of information. Health Aff (Millwood) 31:760–769
Leow JJ, Chang SL, Meyer CP et al (2016) Robot-assisted versus open radical prostatectomy: a contemporary analysis of an all-payer discharge database. Eur Urol 70:837–845
Jeong IG, Khandwala YS, Kim JH et al (2017) Association of robotic-assisted vs laparoscopic radical nephrectomy with perioperative outcomes and health care costs, 2003 to 2015. JAMA 318:1561–1568
Lotan Y (2012) Is robotic surgery cost-effective: no. Curr Opin Urol 22:66–69
Boston-Fleischhauer C (2018) Employers as consumers of healthcare. J Nurs Adm 48:478–480
Epstein AJ, Groeneveld PW, Harhay MO, Yang F, Polsky D (2013) Impact of minimally invasive surgery on medical spending and employee absenteeism. JAMA Surg 148:641–647
Childers CP, Maggard-Gibbons M (2018) Estimation of the acquisition and operating costs for robotic surgery. JAMA 320:835–836
Juo YY, Hyder O, Haider AH, Camp M, Lidor A, Ahuja N (2014) Is minimally invasive colon resection better than traditional approaches?: First comprehensive national examination with propensity score matching. JAMA Surg 149:177–184
Carmichael JC, Keller DS, Baldini G et al (2017) Clinical practice guidelines for enhanced recovery after colon and rectal surgery from the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum 60:761–784
Abeles A, Kwasnicki RM, Darzi A (2017) Enhanced recovery after surgery: current research insights and future direction. World J Gastrointest Surg 9:37–45
Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: a review. JAMA Surg 152:292–298
Hohwu L, Akre O, Pedersen KV, Jonsson M, Nielsen CV, Gustafsson O (2009) Open retropubic prostatectomy versus robot-assisted laparoscopic prostatectomy: a comparison of length of sick leave. Scand J Urol Nephrol 43:259–264
Billfeldt NK, Borgfeldt C, Lindkvist H, Stjerndahl JH, Ankardal M (2018) A Swedish population-based evaluation of benign hysterectomy, comparing minimally invasive and abdominal surgery. Eur J Obstet Gynecol Reprod Biol 222:113–118
Borgfeldt C, Kalapotharakos G, Asciutto KC, Lofgren M, Hogberg T (2016) A population-based registry study evaluating surgery in newly diagnosed uterine cancer. Acta Obstet Gynecol Scand 95:901–911
von Mechow S, Graefen M, Haese A et al (2018) Return to work following robot-assisted laparoscopic and open retropubic radical prostatectomy: a single-center cohort study to compare duration of sick leave. Urol Oncol 36:309.e1-e6
Yaxley JW, Coughlin GD, Chambers SK et al (2016) Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet (London, England) 388:1057–1066
Plym A, Chiesa F, Voss M et al (2016) Work disability after robot-assisted or open radical prostatectomy: a nationwide, population-based study. Eur Urol 70:64–71
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
This study was funded by Intuitive Surgical Inc., which had no involvement in the conduction or reporting of this study. Dr. Quoc-Dien Trinh reports personal fees from Astellas, Bayer and Janssen, outside the submitted work. Dr. Adam S. Kibel reports personal fees from Pfizer, Blue Earth, Merck, Insightec, Profound and Janssen, outside the submitted work. Dr. Daniel Pucheril, Dr. Sean A. Fletcher, Ms. Xi Chen, Dr. David F. Friedlander, Dr. Alexander P. Cole, Dr. Marieke Krimphove, Dr. Adam C. Fields, Dr. Nelya Melnitchouk, and Dr. Prokar Dasgupta have no conflicts of interests or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pucheril, D., Fletcher, S.A., Chen, X. et al. Workplace absenteeism amongst patients undergoing open vs. robotic radical prostatectomy, hysterectomy, and partial colectomy. Surg Endosc 35, 1644–1650 (2021). https://doi.org/10.1007/s00464-020-07547-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07547-y