Abstract
Background
Various training models have been developed for laparoscopic training. Inanimate models including cadavers, ex-vivo simulator, and virtual reality (VR), are less realistic and often fail to display specific events such as bleeding, bile leakage, etc. Animal models provide more realistic experience, but constraints like cost involved, anesthetic requirement, and ethical approval have limited its application. We have designed a new training ex-vivo simulator—Smagister to address these issues.
Methods
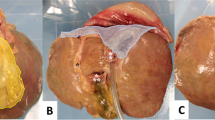
The Smagister consists of a normothermic machine perfusion platform, multivisceral organ of porcine abdominal cavity (liver, gallbladder, pancreas, stomach, intestine, kidney, uterus, bladders, etc.), high-definition display, and software system. Blood gas analysis and number of peristalsis per hour were recorded. A questionnaire was used to subjectively assess vitality of the organ cluster every hour. Three laparoscopic procedures including cholecystectomy (LC), enterotomy closure (LEC) and hepatectomy (LLR) were performed on Smagister, with demonstration of specific events for each procedure. Six experts compared the procedures with actual surgery in terms of feasibility to complete procedures and demonstration of complications.
Results
The fluctuation of perfusate glucose (6.1–8.2 mmol/L) and lactate (5.82–6.55 mmol/L) suggested metabolic function of the multivisceral organs. The mean number of peristalsis was 2.2/min. The simulated surgical view and anatomic structures closely resembled actual surgery during continuous perfusion (3.5 ± 1.0, 3.8 ± 0.8, respectively). The evaluation scores of haptic feedbacks were 3.8 ± 0.8, resembling live tissue handling. LC, LEC, and LLR were performed well on the Smagister, with clear display of the specific events. All six experts considered Smagister as a suitable training modality for both basic and advanced laparoscopic surgery.
Conclusion
The amalgamation of live animal model and ex-vivo simulation in Smagister centralizes the virtue of both modalities, expands the training field, and provides high-fidelity laparoscopic training for both novice and senior surgeons.




Similar content being viewed by others
References
Bang JY, Arnoletti JP, Holt BA, Sutton B, Hasan MK, Navaneethan U, Feranec N, Wilcox CM, Tharian B, Hawes RH, Varadarajulu S (2019) An endoscopic transluminal approach, compared with minimally invasive surgery, reduces complications and costs for patients with necrotizing pancreatitis. Gastroenterology 156:1027–1040.e1023
van Dijk AH, Wennmacker SZ, de Reuver PR, Latenstein CSS, Buyne O, Donkervoort SC, Eijsbouts QAJ, Heisterkamp J, Hof KI, Janssen J, Nieuwenhuijs VB, Schaap HM, Steenvoorde P, Stockmann H, Boerma D, Westert GP, Drenth JPH, Dijkgraaf MGW, Boermeester MA, van Laarhoven C (2019) Restrictive strategy versus usual care for cholecystectomy in patients with gallstones and abdominal pain (SECURE): a multicentre, randomised, parallel-arm, non-inferiority trial. Lancet (Lond, Engl) 393:2322–2330
Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, Belgers EH, van Geloven AA, Gerhards MF, Govaert MJ, van Grevenstein WM, Hoofwijk AG, Kruyt PM, Nienhuijs SW, Boermeester MA, Vermeulen J, van Dieren S, Lange JF, Bemelman WA (2015) Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet (Lond, Engl) 386:1269–1277
Crothers IR, Gallagher AG, McClure N, James DT, McGuigan J (1999) Experienced laparoscopic surgeons are automated to the "fulcrum effect": an ergonomic demonstration. Endoscopy 31:365–369
FuchsWeizman N, Maurer R, Einarsson JI, Vitonis AF, Cohen SL (2015) Survey on barriers to adoption of laparoscopic surgery. J surg educ 72:985–994
Kassab E, Tun JK, Arora S, King D, Ahmed K, Miskovic D, Cope A, Vadhwana B, Bello F, Sevdalis N, Kneebone R (2011) "Blowing up the barriers" in surgical training: exploring and validating the concept of distributed simulation. Ann Surg 254:1059–1065
Mackenzie H, Cuming T, Miskovic D, Wyles SM, Langsford L, Anderson J, Thomas-Gibson S, Valori R, Hanna GB, Coleman MG, Francis N (2015) Design, delivery, and validation of a trainer curriculum for the national laparoscopic colorectal training program in England. Ann Surg 261:149–156
Giger U, Fresard I, Hafliger A, Bergmann M, Krahenbuhl L (2008) Laparoscopic training on thiel human cadavers: a model to teach advanced laparoscopic procedures. Surg Endosc 22:901–906
Wyles SM, Miskovic D, Ni Z, Acheson AG, Maxwell-Armstrong C, Longman R, Cecil T, Coleman MG, Horgan AF, Hanna GB (2011) Analysis of laboratory-based laparoscopic colorectal surgery workshops within the english national training programme. Surg Endosc 25:1559–1566
LeBlanc F, Champagne BJ, Augestad KM, Neary PC, Senagore AJ, Ellis CN, Delaney CP (2010) A comparison of human cadaver and augmented reality simulator models for straight laparoscopic colorectal skills acquisition training. J Am Coll Surg 211:250–255
Cohen J, Cohen SA, Vora KC, Xue X, Burdick JS, Bank S, Bini EJ, Bodenheimer H, Cerulli M, Gerdes H, Greenwald D, Gress F, Grosman I, Hawes R, Mullin G, Schnoll-Sussman F, Starpoli A, Stevens P, Tenner S, Villanueva G (2006) Multicenter, randomized, controlled trial of virtual-reality simulator training in acquisition of competency in colonoscopy. Gastrointest Endosc 64:361–368
Orzech N, Palter VN, Reznick RK, Aggarwal R, Grantcharov TP (2012) A comparison of 2 ex vivo training curricula for advanced laparoscopic skills: a randomized controlled trial. Ann Surg 255:833–839
Gromski MA, Ahn W, Matthes K, De S (2016) Pre-clinical training for new notes procedures: from ex-vivo models to virtual reality simulators. Gastrointest Endosc Clin N Am 26:401–412
Izawa Y, Hishikawa S, Muronoi T, Yamashita K, Maruyama H, Suzukawa M, Lefor AK (2016) Ex-vivo and live animal models are equally effective training for the management of a penetrating cardiac injury. World J Emerg Surg 11:45
BeyerBerjot L, Palter V, Grantcharov T, Aggarwal R (2014) Advanced training in laparoscopic abdominal surgery: a systematic review. Surgery 156:676–688
Palter VN, Orzech N, Aggarwal R, Okrainec A, Grantcharov TP (2010) Resident perceptions of advanced laparoscopic skills training. Surg Endosc 24:2830–2834
Blackburn SC, Griffin SJ (2014) Role of simulation in training the next generation of endoscopists. World J Gastrointest Endosc 6:234–239
Hammoud MM, Nuthalapaty FS, Goepfert AR, Casey PM, Emmons S, Espey EL, Kaczmarczyk JM, Katz NT, Neutens JJ, Peskin EG (2008) To the point: medical education review of the role of simulators in surgical training. Am J Obstet Gynecol 199:338–343
Russell WMS, Burch RL (1959) The principles of humane experimental technique. Methuen & Co Ltd, London
Ceresa CDL, Nasralla D, Knight S, Friend PJ (2017) Cold storage or normothermic perfusion for liver transplantation: probable application and indications. Curr Opin Organ Transplant 22:300–305
He X, Ji F, Zhang Z, Tang Y, Yang L, Huang S, Li W, Su Q, Xiong W, Zhu Z, Wang L, Lv L, Yao J, Zhang L, Zhang L, Guo Z (2018) Combined liver-kidney perfusion enhances protective effects of normothermic perfusion on liver grafts from donation after cardiac death. Liver Transplant 24:67–79
Zhao Q, Huang S, Wang D, Zhang Z, Wu L, Yang L, Ma Y, Ji F, Tang Y, Wang L, Zhu Z, Zhu Y, Xiong W, Chen M, Han M, Zhou J, Hu A, Wang G, Jiao X, Zhu X, Ju W, Guo Z, He X (2018) Does ischemia free liver procurement under normothermic perfusion benefit the outcome of liver transplantation? Ann Transplant 23:258–267
Zhao Q, Nie Y, Guo Z, He X (2019) The future of organ-oriented research and treatment. Hepatobiliary Surg Nutr 8:502–505
Kaneko JJ (2013) Clinical Biochemistry of domestic animals. Academic Press, Cambridge
Liu W, Zheng X, Wu R, Jin Y, Kong S, Li J, Lu J, Yang H, Xu X, Lv Y, Zhang X (2018) Novel laparoscopic training system with continuously perfused ex-vivo porcine liver for hepatobiliary surgery. Surg Endosc 32:743–750
Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, Jarvi KA (2004) The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg 240:374–381
Strickland A, Fairhurst K, Lauder C, Hewett P, Maddern G (2011) Development of an ex vivo simulated training model for laparoscopic liver resection. Surg Endosc 25:1677–1682
Bittner JGT, Coverdill JE, Imam T, Deladisma AM, Edwards MA, Mellinger JD (2008) Do increased training requirements in gastrointestinal endoscopy and advanced laparoscopy necessitate a paradigm shift? A survey of program directors in surgery. J Surg Educ 65:418–430
Acknowledgements
The authors thank the experts for participating in the trial and the staff in Singularity Medicine company for their assistance with setting up the Smagister simulator.
Funding
This study was supported by the National Natural Science Foundation of China (81970564, 81471583 and 81570587), the Guangdong Provincial Key Laboratory Construction Projection on Organ Donation and Transplant Immunology (2013A061401007 and 2017B030314018), Guangdong Provincial Natural Science Funds for Major Basic Science Culture Project (2015A030308010), Guangdong Provincial Natural Science Funds for Distinguished Young Scholars (2015A030306025), Special Support Program for Training High Level Talents in Guangdong Province (2015TQ01R168) and Science and Technology Program of Guangzhou (201704020150).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Xiaobo Wang, Kunsong Zhang, Wenjie Hu, Ming Kuang, Serene Teo, Zhiyong Guo, Qiang Zhao and Xiaoshun He have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, X., Zhang, K., Hu, W. et al. A new platform for laparoscopic training: initial evaluation of the ex-vivo live multivisceral training device. Surg Endosc 35, 374–382 (2021). https://doi.org/10.1007/s00464-020-07411-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07411-z