Abstract
Background
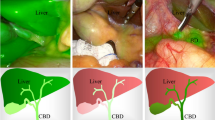
Hepatectomy is a definitive treatment for hepatolithiasis because it simultaneously removes intrahepatic duct (IHD) stones and biliary tract strictures together with the involved liver region en bloc. Unlike cystic or solid liver tumors, hepatolithiasis is usually associated with alterations of anatomical structures and perihepatic adhesions because of chronic recurrent inflammation. This complicates identification of the target hepatic region and location of biliary strictures.
Methods
To determine the efficacy of near-infrared fluorescence (NIRF) imaging using indocyanine green (ICG), we performed a comparative trial and developed a white-light and near-infrared dual-channel image-guided device (DPM-I) for both open and endoscopic surgery. Forty-four eligible patients were randomly assigned to Group A (NIRF imaging) or Group B (traditional hepatectomy). We injected ICG via peripheral veins for patients in Group A.
Results
The NIRF imaging method was associated with less blood loss (OR 1.004, 95% CI 0.999–1.010; P = 0.016), briefer hospitalization (OR 1.336, 95% CI 1.016–1.756; P = 0.001), lower rates of margins with dilated bile ducts (OR 1.278, 95% CI 1.030–1.585; P = 0.023), lower postoperative white blood cell counts (OR 1.262, 95% CI 0.931–1.712; P = 0.038), lower procalcitonin levels (OR 1.316, 95% CI 1.020–1.513; P = 0.002), and lower alanine aminotransferase levels (OR 1.013, 95% CI 1.003–1.023; P = 0.002) compared with traditional hepatectomy.
Conclusions
These data demonstrate the efficacy of NIRF imaging with ICG using DPM-I for treating hepatolithiasis.


Similar content being viewed by others
References
Li EL, Yuan RF, Liao WJ, Feng Q, Lei J, Yin XB, Wu LQ, Shao JH (2019) Intrahepatic bile duct exploration lithotomy is a useful adjunctive hepatectomy method for bilateral primary hepatolithiasis: an eight-year experience at a single centre. BMC Surg 19(1):16
Amar N, Al-Ozaibi L, Badri F (2019) Hepatolithiasis: a case report and literature review. Hamdan Med J 12:86
Peng JX, Wang LZ, Diao JF, Tan ZJ, Zhong XS, Zhen ZP, Chen GH, He JM (2018) Major hepatectomy for primary hepatolithiasis: a comparative study of laparoscopic versus open treatment. Surg Endosc 32:4271–4276
Liu XH, Min XC, Ma Z, He XD, Du ZX (2018) Laparoscopic hepatectomy produces better outcomes for hepatolithiasis than open hepatectomy: an updated systematic review and meta-analysis. Int J Surg 51:151–163
Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, Park JJ, Byun KS, Bak YT (2015) Hepatolithiasis and intrahepatic cholangiocarcinoma: a review. World J Gastroenterol 21:13418–13431
Park HM, Hur YH, Cho CK, Koh YS, Kim HJ, Park EK (2016) Incidence of underlying biliary neoplasm in patients after major hepatectomy for preoperative benign hepatolithiasis. Ann Hepatobiliary Pancreat Surg 20:173–179
Ding GQ, Cai W, Qin MF (2015) Pure laparoscopic versus open liver resection in treatment of hepatolithiasis within the left lobes: a randomized trial study. Surg Laparosc Endosc Percus 25:392–394
Kim YK, Han HS, Yoon YS, Cho JY, Lee W (2015) Laparoscopic approach for right-sided intrahepatic duct stones: a comparative study of laparoscopic versus open treatment. World J Surg 39:1224–1230
Ye XM, Ni KY, Zhou XS, Xie KG, Hong XM (2015) Laparoscopic versus open left hemihepatectomy for hepatolithiasis. J Surg Res 199:402–406
Li EL, Feng Q, Yang QP, Liao WJ, Liu WW, Huang Y, Wu LQ, Yin XB, Shao JH (2017) Effectiveness of hepatic parenchyma lithotomy of hepatolithiasis: a single-center experience. Medicine 96(10):e6134
Shin YC, Jang JY, Kang MJ, Jung W, Chang J, Chang YR, Kim SW (2016) Comparison of laparoscopic versus open left-sided hepatectomy for intrahepatic duct stones. Surg Endosc 30:259–265
Tan JW, Tan YC, Chen F, Zhu YL, Leng JJ, Dong JH (2015) Endoscopic or laparoscopic approach for hepatolithiasis in the era of endoscopy in China. Surg Endosc 29:154–162
Li C, Wen TF (2017) Surgical management of hepatolithiasis: a minireview. Intractable Rare Dis Res 6:102–105
Nguyen QT, Tsien RY (2013) Fluorescence-guided surgery with live molecular navigation—A new cutting edge. Nat Rev Cancer 13:653–662
Nguyen DP, Huber PM, Metzger TA, Genitsch V, Schudel HH, Thalmann GN (2016) A specific mapping study using fluorescence sentinel lymph node detection in patients with intermediate- and high-risk prostate cancer undergoing extended pelvic lymph node dissection. Eur Urol 70:734–737
Ahmed M, Purushotham AD, Douek M (2014) Novel techniques for sentinel lymph node biopsy in breast cancer: a systematic review. Lancet Oncol 15:E351–E362
Sakurai T, Endo M, Shimizu K, Yoshimizu N, Nakajima K, Nosaka K, Dai Y, Iwao A, Jinnai Y (2014) Axillary reverse mapping using fluorescence imaging is useful for identifying the risk group of postoperative lymphedema in breast cancer patients undergoing sentinel node biopsies. J Surg Oncol 109:612–615
van der Vorst JR, Schaafsma BE, Hutteman M, Verbeek FPR, Liefers GJ, Hartgrink HH, Smit V, Lowik C, van de Velde CJH, Frangioni JV, Vahrmeijer AL (2013) Near-infrared fluorescence-guided resection of colorectal liver metastases. Cancer 119:3411–3418
Degett TH, Andersen HS, Gogenur I (2016) Indocyanine green fluorescence angiography for intraoperative assessment of gastrointestinal anastomotic perfusion: a systematic review of clinical trials. Langenbeck Arch Surg 401:767–775
He KS, Zhou J, Yang F, Chi CW, Li H, Mao YM, Hui BG, Wang K, Tian J, Wang J (2018) Near-infrared intraoperative imaging of thoracic sympathetic nerves: from preclinical study to clinical trial. Theranostics 8:304–313
Ishizawa T, Fukushima N, Shibahara J, Masuda K, Tamura S, Aoki T, Hasegawa K, Beck Y, Fukayama M, Kokudo N (2009) Real-time identification of liver cancers by using indocyanine green fluorescent imaging. Cancer 115:2491–2504
Yokoyama N, Otani T, Hashidate H, Maeda C, Katada T, Sudo N, Manabe S, Ikeno Y, Toyoda A, Katayanagi N (2012) Real-time detection of hepatic micrometastases from pancreatic cancer by intraoperative fluorescence imaging preliminary results of a prospective study. Cancer 118:2813–2819
Inoue Y, Arita J, Sakamoto T, Ono Y, Takahashi M, Takahashi Y, Kokudo N, Saiura A (2015) Anatomical liver resections guided by 3-dimensional parenchymal staining using fusion indocyanine green fluorescence imaging. Ann Surg 262:105–111
Mizuno S, Isaji S (2010) Indocyanine green (icg) fluorescence imaging-guided cholangiography for donor hepatectomy in living donor liver transplantation. Am J Transpl 10:2725–2726
Kaibori M, Ishizaki M, Matsui K, Kwon AH (2011) Intraoperative indocyanine green fluorescent imaging for prevention of bile leakage after hepatic resection. Surgery 150:91–98
He KS, Chi CW, Kou DQ, Huang WH, Wu JD, Wang YB, He LF, Ye JZ, Mao YM, Zhang GJ, Wang JD, Tian J (2016) Comparison between the indocyanine green fluorescence and blue dye methods for sentinel lymph node biopsy using novel fluorescence image-guided resection equipment in different types of hospitals. Transl Res 178:74–80
Mao YM, Wang K, He KS, Ye JZ, Yang F, Zhou J, Li H, Chen XY, Wang J, Chi CW, Tian J (2017) Development and application of the near-infrared and white-light thoracoscope system for minimally invasive lung cancer surgery. J Biomed Opt 22(6):66002
Chi C, Du Y, Ye J, Kou D, Qiu J, Wang J, Tian J, Chen X (2014) Intraoperative imaging-guided cancer surgery: from current fluorescence molecular imaging methods to future multi-modality imaging technology. Theranostics 4:1072–1084
Huang LY, Vore M (2001) Multidrug resistance P-glycoprotein 2 is essential for the biliary excretion of indocyanine green. Drug Metab Dispos 29:634–637
De Graaf W, Häusler S, Heger M, van Ginhoven TM, van Cappellen G, Bennink RJ, Kullak-Ublick GA, Hesselmann R, van Gulik TM, Stieger B (2011) Transporters involved in the hepatic uptake of 99mTc-mebrofenin and indocyanine green. J Hepatol 54:738–745
Acknowledgements
This study was supported by the Ministry of Science and Technology of the People’s Republic of China (MOST) (2017YFA0205200, 2017YFA0700401, 2016YFA0100902, 2019YFC0120800), National Natural Science Foundation of China (NSFC) (81527805, 81971773), Key Research Projects in Frontier Science of Chinese Academy of Sciences (CAS) (QYZDJ-SSW-JSC005, KFJ-STS-ZDTP-059), Natural Science Foundation of Guangdong Province of China (2018A0303130292, 2019A1515011356), and Project of Administration of Traditional Chinese Medicine of Guangdong Province of China (20181062), China Postdoctoral Science Foundation (2019M660409). The Clinical Trails was registered with the name of Near-infrared Fluorescence Imaging Applied in Hepatolithiasis with Indocyanine Green, and No. ChiCTR1800020031. http://www.chictr.org.cn/showproj.aspx?proj=32467.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Kunshan He, Xiaopeng Hong, Chongwei Chi, Chaonong Cai, Kun Wang, Peiping Li, Xialei Liu, Jian Li, Hong shan, and Jie Tian have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, K., Hong, X., Chi, C. et al. A new method of near-infrared fluorescence image-guided hepatectomy for patients with hepatolithiasis: a randomized controlled trial. Surg Endosc 34, 4975–4982 (2020). https://doi.org/10.1007/s00464-019-07290-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07290-z