Abstract
Background
Laparoscopic suturing and knot tying is essential for advanced laparoscopic procedures and requires training outside of the operating room. However, personal instruction by experienced surgeons is limitedly available. To address this, the concept of combining e-learning with practical training has become of interest. This study aims to investigate the influence of the first-person perspective in instructional videos, as well as the feasibility of a completely self-directed training curriculum for laparoscopic suturing and knot tying.
Materials and methods
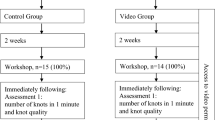
Ninety-one laparoscopically naïve medical students were randomised into two groups training with e-learning videos in either the first-person perspective (combining endoscopic view and view of hands/instruments/forearm motion) or the endoscopic view only. Both groups trained laparoscopic suturing and knot tying in teams of two until reaching predefined proficiency levels. Blinded, trained raters regularly assessed the participants’ performance by using validated checklists. After training, participants filled out questionnaires regarding training experience and personal characteristics.
Results
Average training time to reach proficiency did not differ between groups [first-person perspective (min): 112 ± 44; endoscopic view only (min): 109 ± 47; p = 0.746]. However, participants from both groups perceived the first-person perspective as useful for learning new laparoscopic skills. Both groups showed similar baseline performances and improved significantly after training [Objective Structured Assessment of Technical Skills (OSATS) (max. 37 points): first-person perspective: 30.3 ± 2.3; endoscopic view only: 30.8 ± 2.3]. All participants managed to reach proficiency, needing 8–43 attempts without differences between groups. Visuospatial abilities (mental rotation) seemed to enhance the learning curve.
Conclusion
Modifying instructional videos to the first-person perspective did not translate into a better performance in this setting but was welcomed by participants. Completely self-directed training with the use of e-learning can be a feasible training approach to achieve technical proficiency in laparoscopic suturing and knot tying in a training setting.





Similar content being viewed by others
Abbreviations
- MIS:
-
Minimally invasive surgery
- VR:
-
Virtual reality
- MRT:
-
Mental rotation test
- PSVT: R:
-
Revised purdue spatial visualisation test
References
Dankelman J, Wentink M, Stassen H (2003) Human reliability and training in minimally invasive surgery. Minim Invasive Ther Allied Technol 12:129–135
Stassen H, Dankelman J, Grimbergen K, Meijer D (2001) Man-machine aspects of minimally invasive surgery. Annu Rev Control 25:111–122
Pearson AM, Gallagher AG, Rosser JC, Satava RM (2002) Evaluation of structured and quantitative training methods for teaching intracorporeal knot tying. Surg Endosc 16:130–137
Moulton CA, Dubrowski A, Macrae H, Graham B, Grober E, Reznick R (2006) Teaching surgical skills: what kind of practice makes perfect? A randomized, controlled trial. Ann Surg 244:400–409
Kowalewski KF, Garrow CR, Proctor T, Preukschas AA, Friedrich M, Muller PC, Kenngott HG, Fischer L, Muller-Stich BP, Nickel F (2018) LapTrain: multi-modality training curriculum for laparoscopic cholecystectomy-results of a randomized controlled trial. Surg Endosc 32:3830–3838
Spruit EN, Band GP, Hamming JF, Ridderinkhof KR (2014) Optimal training design for procedural motor skills: a review and application to laparoscopic surgery. Psychol Res 78:878–891
Zevin B, Levy JS, Satava RM, Grantcharov TP (2012) A consensus-based framework for design, validation, and implementation of simulation-based training curricula in surgery. J Am Coll Surg 215(580–586):e583
Stefanidis D, Korndorffer JR Jr, Markley S, Sierra R, Scott DJ (2006) Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 202:599–603
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201:23–29
Stefanidis D, Acker C, Heniford BT (2008) Proficiency-based laparoscopic simulator training leads to improved operating room skill that is resistant to decay. Surg Innov 15:69–73
Wulf G, Shea C, Lewthwaite R (2010) Motor skill learning and performance: a review of influential factors. Med Educ 44:75–84
Whiting H, Den Brinker B (1982) Image of the act. In: Das J, Mulcahy R, Wall A (eds) Theory and research in learning disabilities. Springer, Berlin, pp 217–235
Gallagher AG, O’Sullivan GC (2011) Fundamentals of surgical simulation: principles and practice. Springer, Berlin
Wanzel KR, Ward M, Reznick RK (2002) Teaching the surgical craft: from selection to certification. Curr Probl Surg 39:583–659
Hatala R, Cook DA, Zendejas B, Hamstra SJ, Brydges R (2014) Feedback for simulation-based procedural skills training: a meta-analysis and critical narrative synthesis. Adv Health Sci Educ Theory Pract 19:251–272
Van Bruwaene S, De Win G, Miserez M (2009) How much do we need experts during laparoscopic suturing training? Surg Endosc 23:2755–2761
Xeroulis GJ, Park J, Moulton CA, Reznick RK, Leblanc V, Dubrowski A (2007) Teaching suturing and knot-tying skills to medical students: a randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery 141:442–449
Schmidt MW, Friedrich M, Kowalewski K-F, De La Garza J, Bruckner T, Müller-Stich B-P, Nickel F (2017) Learning from the surgeon’s real perspective—first-person view versus laparoscopic view in e-learning for training of surgical skills? Study protocol for a randomized controlled trial. Int J Surg Protoc 3:7–13
Peters M, Laeng B, Latham K, Jackson M, Zaiyouna R, Richardson C (1995) A redrawn vandenberg and kuse mental rotations test—different versions and factors that affect performance. Brain Cogn 28:39–58
Yoon S (2011) Revised purdue spatial visualization test: visualization of rotations (the revised PSVT: R) [psychometric instrument]. PhD Thesis
Kowalewski KF, Hendrie JD, Schmidt MW, Garrow CR, Bruckner T, Proctor T, Paul S, Adiguzel D, Bodenstedt S, Erben A, Kenngott H, Erben Y, Speidel S, Muller-Stich BP, Nickel F (2017) Development and validation of a sensor- and expert model-based training system for laparoscopic surgery: the iSurgeon. Surg Endosc 31:2155–2165
Moorthy K, Munz Y, Sarker SK, Darzi A (2003) Objective assessment of technical skills in surgery. BMJ 327:1032–1037
Muresan C, Lee TH, Seagull J, Park AE (2010) Transfer of training in the development of intracorporeal suturing skill in medical student novices: a prospective randomized trial. Am J Surg 200:537–541
Chang OH, King LP, Modest AM, Hur H-C (2016) Developing an objective structured assessment of technical skills for laparoscopic suturing and intracorporeal knot tying. J Surg Educ 73:258–263
Romero P, Brands O, Nickel F, Muller B, Gunther P, Holland-Cunz S (2014) Intracorporal suturing–driving license necessary? J Pediatr Surg 49:1138–1141
Schulz KF, Altman DG, Moher D, Group C (2011) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 9:672–677
Schmidt MW, Kowalewski K-F, Schmidt ML, Wennberg E, Garrow CR, Paik S, Benner L, Schijven MP, Müller-Stich BP, Nickel F (2018) The Heidelberg VR Score: development and validation of a composite score for laparoscopic virtual reality training. Surg Endosc. https://doi.org/10.1007/s00464-018-6480-x
Thomson FC, Morrison I, Watson WA (2017) ‘Going Professional’: using point-of-view filming to facilitate preparation for practice in final year medical students. BMJ Simul Technol Enhanc Learn 4:148–149
Bright P, Lord B, Forbes H, Oprescu F, Barr N, Downer T, Phillips NM, McTier L, Simbag V, Alla K (2015) Expert in my pocket: creating first person POV videos to enhance mobile learning. In: THETA 2015: create, connect, consume-innovating today for tomorrow: proceedings of the 2015 the higher education technology agenda conference. THETA, pp 1–15
Fukuta J, Morgan J (2018) First-person perspective video to enhance simulation. Clin Teach 15:231–235
Lynch K, Downer T, Hitchen-Holmes D (2010) Learning in the first person—an initial investigation. In: Proceedings ascilite Sydney
Louridas M, Szasz P, de Montbrun S, Harris KA, Grantcharov TP (2016) Can we predict technical aptitude?: a systematic review. Ann Surg 263:673–691
Roch PJ, Rangnick HM, Brzoska JA, Benner L, Kowalewski K-F, Müller PC, Kenngott HG, Müller-Stich B-P, Nickel F (2018) Impact of visual-spatial ability on laparoscopic camera navigation training. Surg Endosc 32:1174–1183
Hedman L, Klingberg T, Enochsson L, Kjellin A, Felländer-Tsai L (2007) Visual working memory influences the performance in virtual image–guided surgical intervention. Surg Endosc 21:2044–2050
Groenier M, Schraagen JM, Miedema HA, Broeders IA (2014) The role of cognitive abilities in laparoscopic simulator training. Adv Health Sci Educ Theory Pract 19:203–217
Yue J (2004) Spatial visualization by orthogonal rotations. In: Proceedings of ASEE annual conference and exposition, pp 1–10
Rieger U, Pierer K, Farhadi J, Lehmann T, Röers B, Pierer G (2009) Effective acquisition of basic surgical techniques through blended learning. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 80:537–543
Nickel F, Brzoska JA, Gondan M, Rangnick HM, Chu J, Kenngott HG, Linke GR, Kadmon M, Fischer L, Muller-Stich BP (2015) Virtual reality training versus blended learning of laparoscopic cholecystectomy: a randomized controlled trial with laparoscopic novices. Medicine 94:e764
Mittal V, Salem M, Tyburski J, Brocato J (2004) Residents’ working hours in a consortium-wide surgical education program/DISCUSSION. Am Surg 70:127
Strandbygaard J, Bjerrum F, Maagaard M, Winkel P, Larsen CR, Ringsted C, Gluud C, Grantcharov T, Ottesen B, Sorensen JL (2013) Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: a randomized trial. Ann Surg 257:839–844
Trehan A, Barnett-Vanes A, Carty MJ, McCulloch P, Maruthappu M (2015) The impact of feedback of intraoperative technical performance in surgery: a systematic review. BMJ Open 5:e006759
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savović J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Keehner MM, Tendick F, Meng MV, Anwar HP, Hegarty M, Stoller ML, Duh Q-Y (2004) Spatial ability, experience, and skill in laparoscopic surgery. Am J Surg 188:71–75
Wanzel KR, Hamstra SJ, Caminiti MF, Anastakis DJ, Grober ED, Reznick RK (2003) Visual-spatial ability correlates with efficiency of hand motion and successful surgical performance. Surgery 134:750–757
Acknowledgements
This work is part of Ms. Mona W. Schmidt’s doctoral thesis at Heidelberg University. We thank the European Social Fund of the State Baden-Wuerttemberg, from whom we received a total amount of 448.200 € for the laparoscopy training centre at the Department of Surgery at Heidelberg University to conduct laparoscopy training courses and the associated research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mona. W. Schmidt, Karl-Friedrich Kowalewski, Sarah Trent, Laura Benner and Beat-Peter Müller-Stich have no conflict of interest or financial ties to disclose. F. Nickel reports receiving travel support for conference participation as well as equipment provided for laparoscopic surgery courses by KARL STORZ, Johnson & Johnson, Intuitive and Medtronic.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The first two knot of each participant, as well as their last knot after reaching proficiency were recorded on a self-developed and previously validated [21] motion-tracking system. Parameters recorded include duration, path length, angular path length and number of movements. Results can be found in Table 4 in Appendix.
Rights and permissions
About this article
Cite this article
Schmidt, M.W., Kowalewski, KF., Trent, S.M. et al. Self-directed training with e-learning using the first-person perspective for laparoscopic suturing and knot tying: a randomised controlled trial. Surg Endosc 34, 869–879 (2020). https://doi.org/10.1007/s00464-019-06842-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06842-7