Abstract
Introduction
Pre-operative esophagogastroduodenoscopy (EGD) is becoming routine practice in patients undergoing bariatric surgery. Many patients with morbid obesity have obstructive sleep apnea (OSA), which can worsen hypoxia during an EGD. In this study, we report our outcomes using the SuperNO2VA™ device, a sealed nasal positive airway pressure mask designed to deliver high-fraction inhaled oxygen and titratable positive pressure compared to conventional nasal cannula.
Methods
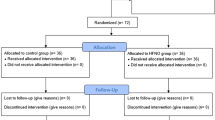
Between June 2016 and August 2017, we conducted a prospective observational study that included 56 consecutive patients who presented for EGD prior to bariatric surgery. Airway management was done using either the SuperNO2VA™ (N = 26) device or conventional nasal cannula (N = 30). Patient demographics, procedure details, and outcomes were compared between the two groups.
Results
The SuperNO2VA™ group had a lower median age compared to the control group (38.5 vs. 48.5 years, p = 0.04). These patients had a higher body mass index (BMI) (47.4 vs. 40.5, IQR, p < 0.0001), higher ASA class (p = 0.03), and were more likely to have OSA (53.9% vs. 26.7%, p = 0.04). Desaturation events were significantly lower in the SuperNO2VA™ group (11.5% vs. 46.7%, p = 0.004) and the median lowest oxygen saturation was higher in the SuperNO2VA™ group (100% vs. 90.5%, p < 0.0001).
Discussion
This is the first study to report on the use of the SuperNO2VA™ device in bariatric patients undergoing pre-operative screening EGD. The use of the SuperNO2VA™ device offers a clinical advantage compared to the current standard of care. Our data demonstrate that patients with higher BMI, higher ASA classification, and OSA were more likely to have the SuperNO2VA™ device used; yet, paradoxically, these patients were less likely to have issues with desaturation events. Use of this device can optimize care in this challenging patient population by minimizing the risks of hypoventilation.

Image taken from https://www.vyaire.com/

Images taken online from https://www.vyaire.com/us/resources/video-gallery?video=283460058
Similar content being viewed by others
References
De Palma GD, Forestieri P (2014) Role of endoscopy in the bariatric surgery of patients. World J Gastroenterol 20(24):7777–7784. https://doi.org/10.3748/wjg.v20.i24.7777
Early DS, Lightdale JR, Vargo JJ et al (2018) Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc 87(2):327–337. https://doi.org/10.1016/j.gie.2017.07.018
American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists (2002) Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology 96(4):1004–1017
Coté GA, Hovis RM, Ansstas MA et al (2010) Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol 8(2):137–142. https://doi.org/10.1016/j.cgh.2009.07.008
Yilmaz M, Aydin A, Karasu Z, Günşar F, Ozütemiz O (2002) Risk factors associated with changes in oxygenation and pulse rate during colonoscopy. Turk J Gastroenterol 13(4):203–208
Friedrich-Rust M, Welte M, Welte C et al (2014) Capnographic monitoring of propofol-based sedation during colonoscopy. Endoscopy 46(3):236–244. https://doi.org/10.1055/s-0033-1359149
Mehta PP, Kochhar G, Albeldawi M et al (2016) Capnographic monitoring in routine EGD and colonoscopy with moderate sedation: a prospective, randomized, controlled trial. Am J Gastroenterol 111(3):395–404. https://doi.org/10.1038/ajg.2015.437
Committee on Standards and Practice Parameters. Standards for basic anesthetic monitoring. https://www.asahq.org/standards-and-guidelines/standards-for-basic-anesthetic-monitoring. Accessed 28 Jan 2019
Schumann R, Natov NS, Rocuts-Martinez KA et al (2016) High-flow nasal oxygen availability for sedation decreases the use of general anesthesia during endoscopic retrograde cholangiopancreatography and endoscopic ultrasound. World J Gastroenterol 22(47):10398–10405. https://doi.org/10.3748/wjg.v22.i47.10398
Patel A, Nouraei SAR (2015) Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia 70(3):323–329. https://doi.org/10.1111/anae.12923
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Dimou, Dakin, Turnbull, Pomp, Samuels, Afaneh, and Ms. Huynh have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dimou, F., Huynh, S., Dakin, G. et al. Nasal positive pressure with the SuperNO2VA™ device decreases sedation-related hypoxemia during pre-bariatric surgery EGD. Surg Endosc 33, 3828–3832 (2019). https://doi.org/10.1007/s00464-019-06721-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06721-1