Abstract
Background
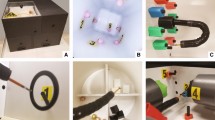
Objective assessment of endoscopist competency is important. Recently, the endoscopic part-task training box (Thompson Endoscopic Skills Trainer [TEST]) was developed to assess endoscopist competency. We aimed to evaluate the ability of the TEST to assess competency during endoscopic procedures, especially endoscopic submucosal dissection (ESD).
Methods
Twenty-three physicians were included in this study. Correlations between TEST scores and the following factors were evaluated: years of endoscopic experience, number of esophagogastroduodenoscopies (EGDs) performed, number of colonoscopies (CSs) performed, cecal intubation rate, number of gastric ESDs performed, gastric ESD procedure time/lesion size (min/mm2), and gastric ESD self-completion rate. Also, correlation coefficients between the number of gastric ESDs performed and each of gastric ESD procedure time/lesion size and gastric ESD self-completion rate were calculated.
Results
TEST scores showed strong correlations to different factors: years of experience in endoscopy: 0.957 (p < 0.01); number of EGDs: 0.947 (p < 0.01); number of CSs: 0.947, (p < 0.01); number of gastric ESDs: 0.924 (p < 0.01); gastric ESD procedure time/lesion size: − 0.9 (p < 0.01); self-completion rate of gastric ESDs: 0.857 (p < 0.005). The number of gastric ESDs performed was not more strongly correlated to procedure time of gastric ESDs or self-completion rate of gastric ESDs compared to TEST scores (− 0.824 (p < 0.01) and 0.704 (p < 0.05), respectively). TEST scores of endoscopists with a cecal intubation rate ≥ 90% were > 380, while the scores of physicians with a gastric ESD self-completion rate ≥ 90% were > 700.
Conclusions
TEST score correlates with both basic and advanced endoscopic procedures. TEST is therefore a promising option for assessing endoscopist competency, and might be useful for providing threshold scores as competency markers for specific endoscopic procedures such as gastric ESD.





Similar content being viewed by others
References
Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, Fanelli RD, Wheeler-Harbough J, American Society for Gastrointestinal Endoscopy (2002) Methods of granting hospital privileges to perform gastrointestinal endoscopy. Gastrointest Endosc 55:780–783
Cass OW (1999) Training to competence in gastrointestinal endoscopy: a plea for continuous measuring of objective end points. Endoscopy 31:751–754. https://doi.org/10.1055/s-1999-148
Shahidi N, Ou G, Telford J, Enns R (2014) Establishing the learning curve for achieving competency in performing colonoscopy: a systematic review. Gastrointest Endosc 80:410–416. https://doi.org/10.1016/j.gie.2014.04.056
Shahidi N, Ou G, Telford J, Enns R (2015) When trainees reach competency in performing ERCP: a systematic review. Gastrointest Endosc 81:1337–1342. https://doi.org/10.1016/j.gie.2014.12.054
Training Committee ASGE, Sedlack RE, Coyle WJ, Obstein KL, Al-Haddad MA, Bakis G, Christie JA, Davila RE, DeGregorio B, DiMaio CJ, Enestvedt BK, Jorgensen J, Mullady DK, Rajan L (2014) ASGE’s assessment of competency in endoscopy evaluation tools for colonoscopy and EGD. Gastrointest Endosc 79:1–7. https://doi.org/10.1016/j.gie.2013.10.003
Sedlack RE (2011) Training to competency in colonoscopy: assessing and defining competency standards. Gastrointest Endosc 74:355–366. https://doi.org/10.1016/j.gie.2011.02.019
Vassiliou MC, Dunkin BJ, Fried GM, Mellinger JD, Trus T, Kaneva P, Lyons C, Korndorffer JR Jr, Ujiki M, Velanovich V, Kochman ML, Tsuda S, Martinez J, Scott DJ, Korus G, Park A, Marks JM (2014) Fundamentals of endoscopic surgery: creation and validation of the hands-on test. Surg Endosc 28:704–711. https://doi.org/10.1007/s00464-013-3298-4
Poulose BK, Vassiliou MC, Dunkin BJ, Mellinger JD, Fanelli RD, Martinez JM, Hazey JW, Sillin LF, Delaney CP, Velanovich V, Fried GM, Korndorffer JR Jr, Marks JM (2014) Fundamentals of endoscopic surgery cognitive examination: development and validity evidence. Surg Endosc 28:631–638. https://doi.org/10.1007/s00464-013-3220-0
Hazey JW, Marks JM, Mellinger JD, Trus TL, Chand B, Delaney CP, Dunkin BJ, Fanelli RD, Fried GM, Martinez JM, Pearl JP, Poulose BK, Sillin LF, Vassiliou MC, Melvin WS (2014) Why fundamentals of endoscopic surgery (FES)? Surg Endosc 28:701–703. https://doi.org/10.1007/s00464-013-3299-3
Jirapinyo P, Thompson CC (2015) Current status of endoscopic simulation in gastroenterology fellowship training programs. Surg Endosc 29:1913–1919. https://doi.org/10.1007/s00464-014-3884-0
Jirapinyo P, Kumar N, Thompson CC (2015) Validation of an endoscopic part-task training box as a skill assessment tool. Gastrointest Endosc 81:967–973. https://doi.org/10.1016/j.gie.2014.08.007
Thompson CC, Jirapinyo P, Kumar N, Ou A, Camacho A, Lengyel B, Ryan MB (2014) Development and initial validation of an endoscopic part-task training box. Endoscopy 46:735–744. https://doi.org/10.1055/s-0034-1365463
Goda K, Fujishiro M, Hirasawa K, Kakushima N, Morita Y, Oda I, Takeuchi M, Yamamoto Y, Uedo N (2012) How to teach and learn endoscopic submucosal dissection for upper gastrointestinal neoplasm in Japan. Dig Endosc 24(Suppl 1):136–142, https://doi.org/10.1111/j.1443-1661.2012.01274.x
Yamamoto S, Uedo N, Ishihara R, Kajimoto N, Ogiyama H, Fukushima Y, Yamamoto S, Takeuchi Y, Higashino K, Iishi H, Tatsuta M (2009) Endoscopic submucosal dissection for early gastric cancer performed by supervised residents: assessment of feasibility and learning curve. Endoscopy 41:923–928. https://doi.org/10.1055/s-0029-1215129
Bhatt A, Abe S, Kumaravel A, Parsi MA, Stevens T, Jang S, Lopez R, Oda I, Vargo JJ, Saito Y (2016) Video-based supervision for training of endoscopic submucosal dissection. Endoscopy 48:711–716. https://doi.org/10.1055/s-0042-106722
Author information
Authors and Affiliations
Contributions
NT: conception and design; analysis and interpretation of the data; drafting of the article. HA: conception and design; critical revision of the article for important intellectual content. MK: conception and design. KI: conception and design. KS: conception and design.
Corresponding author
Ethics declarations
Disclosures
Naoto Tamai, Hiroyuki Aihara, Masayuki Kato, Kimio Isshi, and Kazuki Sumiyama have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Tamai, N., Aihara, H., Kato, M. et al. Competency assessment for gastric endoscopic submucosal dissection using an endoscopic part-task training box. Surg Endosc 33, 2548–2552 (2019). https://doi.org/10.1007/s00464-018-6548-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6548-7