Abstract
Background
Improvement in morbidity of pancreatoduodenectomy (PD) largely depends on the reduction in the incidence of clinically relevant (CR) postoperative pancreatic fistula (POPF).
Methods
After internal validation of the clinical risk score (CRS) of POPF, and identification of other predictive factors for POPF, robotic (RPD), and open (OPD) PDs were stratified into risk categories and matched by propensity scores. The primary endpoint of this study was incidence of CR-POPF. Secondary endpoints were 90-day morbidity and mortality, and sample size calculation for randomized controlled trials (RCT).
Results
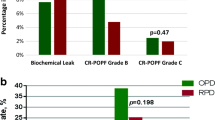
No patient undergoing RPD was classified at negligible risk for POPF, and no CR-POPF occurred in 7 RPD at low risk. The matching process identified 48 and 11 pairs at intermediate and high risk for POPF, respectively. In the intermediate-risk group, RPD was associated with higher rates of CR-POPF (31.3% vs 12.5%) (p = 0.0026), with equivalent incidence of grade C POPF. In the high-risk group, CR-POPF occurred frequently, but in similar percentages, after either procedures. Starting from an unadjusted point estimate of the effect size of 1.71 (0.91–3.21), the pair-matched odds ratio for CR-POPF after RPD was 2.80 (1.01–7.78) for the intermediate-risk group, and 0.20 (0.01–4.17) for the high-risk group. Overall morbidity and mortality were equivalent in matched study groups. Sample size calculation for a non-inferiority RCT demonstrated that a total of 31,669 PDs would be required to randomize 682 patients at intermediate risk and 1852 patients at high risk.
Conclusions
In patients at intermediate risk, RPD is associated with higher rates of CR-POPF. Incidence of grade C POPF is similar in RPD and OPD, making overall morbidity and mortality also equivalent. A RCT, with risk stratification for POPF, would require an enormous number of patients. Implementation of an international registry could be the next step in the assessment of RPD.



Similar content being viewed by others
References
Kelley WE (2008) The evolution of laparoscopy and the revolution in surgery in the decade of the 1990s. JSLS 12:351–357
Allori AC, Leitman IM, Heitman E (2010) Delayed assessment and eager adoption of laparoscopic cholecystectomy: implications for developing surgical technologies. World J Gastroenterol 16:4115–4122
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, COLOR II Study Group (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Ni M, Mackenzie H, Widdison A, Jenkins JT, Mansfield S, Dixon T, Slade D, Coleman MG, Hanna GB (2016) What errors make a laparoscopic cancer surgery unsafe? An ad hoc analysis of competency assessment in the National Training Programme for laparoscopic colorectal surgery in England. Surg Endosc 30:1020–1027
Nanidis TG, Antcliffe D, Kokkinos C, Borysiewicz CA, Darzi AW, Tekkis PP, Papalois VE (2008) Laparoscopic versus open live donor nephrectomy in renal transplantation: a meta-analysis. Ann Surg 247:58–70
Shrikhande SV, Sivasanker M, Vollmer CM, Friess H, Besselink MG, Fingerhut A, Yeo CJ, Fernandez-delCastillo C, Dervenis C, Halloran C, Gouma DJ, Radenkovic D, Asbun HJ, Neoptolemos JP, Izbicki JR, Lillemoe KD, Conlon KC, Fernandez-Cruz L, Montorsi M, Bockhorn M, Adham M, Charnley R, Carter R, Hackert T, Hartwig W, Miao Y, Sarr M, Bassi C, Büchler MW, International Study Group of Pancreatic Surgery (ISGPS) (2017) Pancreatic anastomosis after pancreatoduodenectomy: a position statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 161:584–591
Vollmer CM Jr, Sanchez N, Gondek S, McAuliffe J, Kent TS, Christein JD et al (2012) A root-cause analysis of mortality following major pancreatectomy. J Gastrointest Surg 16:89–102
Gawlas I, Sethi M, Winner M, Epelboym I, Lee JL, Schrope BA, Chabot JA, Allendorf JD (2013) Readmission after pancreatic resection is not an appropriate measure of quality. Ann Surg Oncol 20:1781–1787
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8:408–410
Gagner M, Palermo M (2009) Laparoscopic Whipple procedure: review of the literature. J Hepatobiliary Pancreat Surg 16:726–730
Boggi U, Amorese G, Vistoli F, Caniglia F, De Lio N, Perrone V, Barbarello L, Belluomini M, Signori S, Mosca F (2015) Laparoscopic pancreaticoduodenectomy: a systematic literature review. Surg Endosc 29:9–23
McMillan MT, Zureikat AH, Hogg ME, Kowalsky SJ, Zeh HJ, Vollmer Sprys MH, Jr CM (2017) A propensity score-matched analysis of robotic vs open pancreatoduodenectomy on incidence of pancreatic fistula. JAMA Surg 152:327–335
Adam MA, Choudhury K, Dinan MA, Reed SD, Scheri RP, Blazer DG 3rd, Roman SA, Sosa JA (2015) Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg 262:372–377
Chen S, Chen JZ, Zhan Q, Deng XX, Shen BY, Peng CH, Li HW (2015) Robot-assisted laparoscopic versus open pancreaticoduodenectomy: a prospective, matched, mid-term follow-up study. Surg Endosc 29:3698–3711
Wellner UF, Küsters S, Sick O, Busch C, Bausch D, Bronsert P, Hopt UT, Karcz KW, Keck T (2014) Hybrid laparoscopic versus open pylorus-preserving pancreatoduodenectomy: retrospective matched case comparison in 80 patients. Langenbecks Arch Surg 399:849–856
Bao PQ, Mazirka PO, Watkins KT (2014) Retrospective comparison of robot-assisted minimally invasive versus open pancreaticoduodenectomy for periampullary neoplasms. J Gastrointest Surg 18:682–689
Chalikonda S, Aguilar-Saavedra JR, Walsh RM (2012) Laparoscopic robotic-assisted pancreaticoduodenectomy: a case-matched comparison with open resection. Surg Endosc 26:2397–2402
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr (2013) A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg 216:1–14
Miller BC, Christein JD, Behrman SW, Drebin JA, Pratt WB, Callery MP, Vollmer CM Jr (2014) A multi-institutional external validation of the fistula risk score for pancreatoduodenectomy. J Gastrointest Surg 18:172–179
Shubert CR, Wagie AE, Farnell MB, Nagorney DM, Que FG, Lombardo KMR, Truty MJ, Smoot RL, Kendrick ML (2015) Clinical risk score to predict pancreatic fistula after pancreatoduodenectomy: independent external validation for open and laparoscopic approaches. J Am Coll Surg 221:689–698
Polanco PM, Zenati MS, Hogg ME, Shakir M, Boone BA, Barlett DL, Zeh HJ, Zureikat AH (2016) An analysis of risk factors for pancreatic fistula after robotic pancreaticoduodenectomy: outcomes from a consecutive series of standardized pancreatic reconstructions. Surg Endosc 30:1523–1529
Boggi U, Signori S, De Lio N, Perrone VG, Vistoli F, Belluomini M, Cappelli C, Amorese G, Mosca F (2013) Feasibility of robotic pancreaticoduodenectomy. Br J Surg 100:917–925
Mucksavage P, Kerbl DC, Lee JY (2011) The da Vinci® Surgical System overcomes innate hand dominance. J Endourol 25:1385–1388
Mise Y, Vauthey JN, Zimmitti G, Parker NH, Conrad C, Aloia TA, Lee JE, Fleming JB, Katz MH (2015) Ninety-day postoperative mortality is a legitimate measure of hepatopancreatobiliary surgical quality. Ann Surg 262:1071–1078
Swanson RS, Pezzi CM, Mallin K, Loomis AM, Winchester DP (2014) The 90-day mortality after pancreatectomy for cancer is double the 30-day mortality: more than 20,000 resections from the national cancer data base. Ann Surg Oncol 21:4059–4067
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M, for the International Study Group on Pancreatic Fistula (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Pancreas Club Calculator ISGPS leak definition. Available at: http://pancreasclub.com/calculators/isgps-calculator/
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142:761–768
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW (2007) Postpancreatectomy hemorrhage (PPH)—an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142:20–25
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58:277–280
Song KB, Kim SC, Hwang DW, Lee JH, Lee DJ, Lee JW, Park KM, Lee YJ (2015) Matched case-control analysis comparing laparoscopic and open pylorus-preserving pancreaticoduodenectomy in patients with periampullary tumors. Ann Surg 262:146–155
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Petermann D, Demartines N, Schäfer M (2013) Severe postoperative complications adversely affect long-term survival after R1 resection for pancreatic head adenocarcinoma. World J Surg 37:1901–1908
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Napoli N, Kauffmann EF, Menonna F, Perrone VG, Brozzetti S, Boggi U (2016) Indications technique and results of robotic pancreatoduodenectomy. Updates Surg 68:295–305
Kauffmann EF, Napoli N, Menonna F, Vistoli F, Amorese G, LE Campani Pollina, Funel N, Cappelli C, Caramella D, Boggi U (2016) Robotic pancreatoduodenectomy with vascular resection. Langenbecks Arch Surg 401:1111–1122
Boggi U, Napoli N, Costa F, Kauffmann EF, Menonna F, Iacopi S, Vistoli F, Amorese G (2016) Robotic pancreatic resections. World J Surg 40:2497–2506
Napoli N, Kauffmann EF, Palmeri M, Miccoli M, Costa F, Vistoli F, Amorese G, Boggi U (2016) The learning curve in robotic pancreatoduodenectomy. Dig Surg 33:299–307
Kang CM, Kim DH, Lee WJ (2010) Ten years of experience with resection of left-sided pancreatic ductal adenocarcinoma: evolution and initial experience to a laparoscopic approach. Surg Endosc 24:1533–1541
Pratt WB, Maithel SK, Vanounou T, Huang ZS, Callery MP, Vollmer CM Jr (2007) Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme. Ann Surg 245:443–451
Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, Kendrick ML (2014) Total laparoscopic pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic advantages over open approaches? Ann Surg 260:633–638 (discussion 638–40)
Zureikat AH, Moser AJ, Boone BA, Bartlett DL, Zenati M, Zeh HJ 3rd (2013) 250 robotic pancreatic resections: safety and feasibility. Ann Surg 258:554–559 (discussion 559–62)
Strobel O, Büchler MW (2015) Increased mortality due to lack of experience with minimally invasive pancreatoduodenectomy. Chirurg 86:496
de la Fuente SG (2013) Laparoscopic pancreaticoduodenectomies: a word of caution. J Am Coll Surg 216:1218
Zureikat AH, Nguyen KT, Bartlett DL, Zeh HJ, Moser AJ (2011) Robotic-assisted major pancreatic resection and reconstruction. Arch Surg 146:256–261
McMillan MT, Soi S, Asbun HJ, Ball CG, Bassi C, Beane JD, Behrman SW, Berger AC, Bloomston M, Callery MP, Christein JD, Dixon E, Drebin JA, Fernandez-del Castillo C, Fisher WE, Ven Fong Z, House MG, Hughes SJ, Kent TS, Kunstman JW, Malleo G, Miller BC, Salem RR, Soares K, Valero V, Wolfgang CL, Vollmer CM (2016) Risk-adjusted outcomes of clinically relevant pancreatic fistula following pancreatoduodenectomy: a model for performance evaluation. Ann Surg 264:344–352
Dokmak S, Ftériche FS, Aussilhou B, Bensafta Y, Lévy P, Ruszniewski P (2015) Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 220:831–838
Fujii T, Sugimoto H, Yamada S, Kanda M, Suenaga M, Takami H, Hattori M, Inokawa Y, Nomoto S, Fujiwara M, Kodera Y (2014) Modified Blumgart anastomosis for pancreaticojejunostomy: technical improvement in matched historical control study. J Gastrointest Surg 18:1108–1115
Poves I, Morató O, Burdío F, Grande L (2017) Laparoscopic-adapted Blumgart pancreaticojejunostomy in laparoscopic pancreaticoduodenectomy. Surg Endosc 31:2837–2845
Halloran CM, Platt K, Gerard A, Polydoros F, O’Reilly DA, Gomez D, Smith A, Neoptolemos JP, Soonwalla Z, Taylor M, Blazeby JM, Ghaneh P (2016) PANasta Trial; Cattell Warren versus Blumgart techniques of panreatico-jejunostomy following pancreato-duodenectomy: study protocol for a randomized controlled trial. Trials 17:30
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Niccolò Napoli, Emanuele Federico Kauffmann, Francesca Menonna, Francesca Costa, Sara Iacopi, Gabriella Amorese, Serena Giorgi, Angelo Baggiani, and Ugo Boggi have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Napoli, N., Kauffmann, E.F., Menonna, F. et al. Robotic versus open pancreatoduodenectomy: a propensity score-matched analysis based on factors predictive of postoperative pancreatic fistula. Surg Endosc 32, 1234–1247 (2018). https://doi.org/10.1007/s00464-017-5798-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5798-0