Abstract
Objective
To investigate the risk of incisional hernia repair (IHR) and paracolostomy hernia repair (PHR) following open and laparoscopic rectal cancer resection with curative intent.
Background
Laparoscopic rectal cancer resection has been implemented to varying degrees around the world. IHR and PHR following open and laparoscopic rectal cancer resection have only been sparingly evaluated.
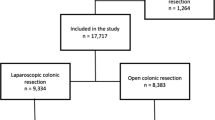
Methods
Patients who underwent rectal cancer resection were identified in the Danish Colorectal Cancer Group’s database. To identify IHR and PHR following rectal cancer resection, we linked data to the Danish Ventral Hernia Database. The absolute risk of IHR and PHR was estimated as cumulative incidence proportions, treating death as competing risk. We used Cox proportional hazard regression analysis with multivariable adjustment to compute hazard ratios (HRs) comparing open and laparoscopic approach.
Results
The 5-year risk of IHR was 4.1% among patients undergoing open resection (n = 3090) and 3.2% among those undergoing laparoscopic resection (n = 3099), corresponding to a risk difference of 0.9% (95% CI 0.0–2.0, P = 0.057). Laparoscopic rectal resection was not associated with lower risk of IHR (adjusted HR 0.94, 95% CI 0.67–1.31, P = 0.709). A total of 2577 patients had a colostomy at rectal cancer resection and the 5-year risk of PHR was 2.1% after open surgery compared with 6.7% after laparoscopic surgery, corresponding to a risk difference of −4.6% (95% CI −6.4 to −2.7, P < 0.001). Laparoscopic surgery was associated with increased risk of PHR (adjusted HR 2.56, 95% CI 1.53–4.29, P < 0.001).
Conclusion
We observed no association between surgical approach of rectal cancer resection and subsequent IHR. Laparoscopic surgery was associated with increased risk of PHR.

Similar content being viewed by others
References
Korenkov M, Paul A, Sauerland S, Neugebauer E, Arndt M, Chevrel JP, Corcione F, Fingerhut A, Flament JB, Kux M, Matzinger A, Myrvold HE, Rath AM, Simmermacher RK (2001) Classification and surgical treatment of incisional hernia. Results of an experts’ meeting. Langenbecks Arch Surg 386:65–73
Kingsnorth A, LeBlanc K (2003) Hernias: inguinal and incisional. Lancet 362:1561–1571. doi:10.1016/S0140-6736(03)14746-0
Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A, Davies L, Glasbey JC, Frewer KA, Frewer NC, Russell D, Russell I, Torkington J (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14 618 patients. PLoS ONE 10:e0138745. doi:10.1371/journal.pone.0138745
Nieuwenhuizen J, Kleinrensink GJ, Hop WC, Jeekel J, Lange JF (2008) Indications for incisional hernia repair: an international questionnaire among hernia surgeons. Hernia 12:223–225. doi:10.1007/s10029-007-0322-4
Israelsson LA (2005) Preventing and treating parastomal hernia. World J Surg 29:1086–1089. doi:10.1007/s00268-005-7973-z
Nikberg M, Sverrisson I, Tsimogiannis K, Chabok A, Smedh K (2015) Prophylactic stoma mesh did not prevent parastomal hernias. Int J Colorectal Dis 30:1217–1222. doi:10.1007/s00384-015-2293-8
Gregg ZA, Dao HE, Schechter S, Shah N (2014) Paracolostomy hernia repair: who and when? J Am Coll Surg 218:1105–1112. doi:10.1016/j.jamcollsurg.2014.01.054
The Danish Colorectal Cancer Database (2015) Annu Rev 2014:2016
Vennix S, Pelzers L, Bouvy N, Beets GL, Pierie JP, Wiggers T, Breukink S (2014) Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database Syst Rev 4:CD005200. doi:10.1002/14651858.CD005200.pub3
Le Huu Nho R, Mege D, Ouaissi M, Sielezneff I, Sastre B (2012) Incidence and prevention of ventral incisional hernia. J Visc Surg 149:e3–e14. doi:10.1016/j.jviscsurg.2012.05.004
Burns EM, Currie A, Bottle A, Aylin P, Darzi A, Faiz O (2013) Minimal-access colorectal surgery is associated with fewer adhesion-related admissions than open surgery. Br J Surg 100:152–159. doi:10.1002/bjs.8964
Bartels SA, Vlug MS, Hollmann MW, Dijkgraaf MG, Ubbink DT, Cense HA, van Wagensveld BA, Engel AF, Gerhards MF, Bemelman WA, Collaborative LAFA Study Group (2014) Small bowel obstruction, incisional hernia and survival after laparoscopic and open colonic resection (LAFA study). Br J Surg 101:1153–1159. doi:10.1002/bjs.9585
Klaristenfeld DD, McLemore EC, Li BH, Abbass MA, Abbas MA (2015) Significant reduction in the incidence of small bowel obstruction and ventral hernia after laparoscopic compared to open segmental colorectal resection. Langenbecks Arch Surg 400:505–512. doi:10.1007/s00423-015-1301-3
Ng SS, Leung KL, Lee JF, Yiu RY, Li JC, Hon SS (2009) Long-term morbidity and oncologic outcomes of laparoscopic-assisted anterior resection for upper rectal cancer: ten-year results of a prospective, randomized trial. Dis Colon Rectum 52:558–566. doi:10.1007/DCR.0b013e31819ec20c
Mishra A, Keeler B, Maxwell-Armstrong C, Simpson A, Acheson A (2014) The influence of laparoscopy on incisional hernia rates: a retrospective analysis of 1057 colorectal cancer resections. Colorectal Dis. doi:10.1111/codi.12687
Pedersen CB (2011) The Danish civil registration system. Scand J Public Health 39:22–25. doi:10.1177/1403494810387965
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scand J Public Health 39:30–33. doi:10.1177/1403494811401482
Danish Ventral Hernia Database (2014) Annual report 2014. Available at: https://www.sundhed.dk/content/cms/97/4697_hernie_%C3%A5rsrapport2014_endelig.pdf. 2016; Accessed 19 Jun 2016
Helgstrand F, Tenma J, Rosenberg J, Kehlet H, Bisgaard T (2013) High agreement between the Danish Ventral Hernia Database and hospital files. Dan Med J 60:A4708
Iversen LH, Ingeholm P, Gogenur I, Laurberg S (2014) Major reduction in 30-day mortality after elective colorectal cancer surgery: a nationwide population-based study in Denmark 2001–2011. Ann Surg Oncol 21:2267–2273. doi:10.1245/s10434-014-3596-7
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT (2011) The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 11:83. doi:10.1186/1471-2288-11-83
Kim HT (2007) Cumulative incidence in competing risks data and competing risks regression analysis. Clin Cancer Res 13:559–565
White IR, Royston P, Wood AM (2011) Multiple imputation using chained equations: issues and guidance for practice. Stat Med 30:377–399. doi:10.1002/sim.4067
Andersen LP, Klein M, Gogenur I, Rosenberg J (2008) Incisional hernia after open versus laparoscopic sigmoid resection. Surg Endosc 22:2026–2029. doi:10.1007/s00464-008-9924-x
Laurent C, Leblanc F, Bretagnol F, Capdepont M, Rullier E (2008) Long-term wound advantages of the laparoscopic approach in rectal cancer. Br J Surg 95:903–908. doi:10.1002/bjs.6134
Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, Leitman IM (2010) Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg 200:265–269. doi:10.1016/j.amjsurg.2009.08.044
Taylor GW, Jayne DG, Brown SR, Thorpe H, Brown JM, Dewberry SC, Parker MC, Guillou PJ (2010) Adhesions and incisional hernias following laparoscopic versus open surgery for colorectal cancer in the CLASICC trial. Br J Surg 97:70–78. doi:10.1002/bjs.6742
Kokotovic D, Sjolander H, Gogenur I, Helgstrand F (2016) Watchful waiting as a treatment strategy for patients with a ventral hernia appears to be safe. Hernia. doi:10.1007/s10029-016-1464-z
Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T (2012) Reoperation versus clinical recurrence rate after ventral hernia repair. Ann Surg 256:955–958. doi:10.1097/SLA.0b013e318254f5b9
Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T (2013) Outcomes after emergency versus elective ventral hernia repair: a prospective nationwide study. World J Surg 37:2273–2279. doi:10.1007/s00268-013-2123-5
Timmermans L, Deerenberg EB, Lamme B, Jeekel J, Lange JF (2014) Parastomal hernia is an independent risk factor for incisional hernia in patients with end colostomy. Surgery 155:178–183. doi:10.1016/j.surg.2013.06.014
Rosen MJ, Reynolds HL, Champagne B, Delaney CP (2010) A novel approach for the simultaneous repair of large midline incisional and parastomal hernias with biological mesh and retrorectus reconstruction. Am J Surg 199:416–420. doi:10.1016/j.amjsurg.2009.08.026 discussion 420-421
Aquina CT, Probst CP, Becerra AZ, Iannuzzi JC, Hensley BJ, Noyes K, Monson JR, Fleming FJ (2015) Missed opportunity: laparoscopic colorectal resection is associated with lower incidence of small bowel obstruction compared to an open approach. Ann Surg. doi:10.1097/SLA.0000000000001389
Funding
This study was supported by the Program for Clinical Research Infrastructure (PROCRIN Grant No. R1-005) established by the Lundbeck Foundation and the Novo Nordisk Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Rune Erichsen, Trine Frøslev, and Lene H. Iversen were supported by the Program for Clinical Research Infrastructure (PROCRIN) established by the Lundbeck Foundation and the Novo Nordisk Foundation. Drs. Peter Andersen, Mogens R. Madsen, and Søren Laurberg have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Andersen, P., Erichsen, R., Frøslev, T. et al. Open versus laparoscopic rectal cancer resection and risk of subsequent incisional hernia repair and paracolostomy hernia repair: a nationwide population-based cohort study. Surg Endosc 32, 134–144 (2018). https://doi.org/10.1007/s00464-017-5648-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5648-0