Abstract
Background
Simulators are useful tools in the development of laparoscopic skills. However, little is known about the effectiveness of short laparoscopic training sessions and how retention of skills occurs in surgical trainees who are naïve to laparoscopy. This study analyses the retention of laparoscopic surgical skills in medical students without prior surgical training.
Methods
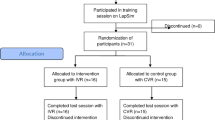
A group of first- and second-year medical students (n = 68), without prior experience in surgery or laparoscopy, answered a demographic questionnaire and had their laparoscopic skills assessed by the Fundamentals of Laparoscopic Surgery (FLS) training protocol. Subsequently, they underwent a 150-minute training course after which they were re-tested. One year after the training, the medical students’ performance in the simulator was re-evaluated in order to analyse retention.
Results
Of the initial 68 students, a total of 36 participated throughout the entire study, giving a final participation rate of 52 %. Thirty-six medical students with no gender predominance and an average age of 20 years were evaluated. One year after the short training programme, retention was 69.3 % in the peg transfer (p < 0.05) and 64.2 % in ligature (p < 0.05) compared with immediate post-training evaluation. There was no significant difference in suturing. The average sample score in the baseline test was 8.3, in the post-training test it was 89.7, and in the retention test it was 84.2, which corresponded to a skill retention equivalence of 93 %.
Conclusions
There was a significant retention of the laparoscopic surgical skills developed. Even 1 year after a short training session, medical students without previous surgical experience showed that they have retained a great part of the skills acquired through training.


Similar content being viewed by others
Abbreviations
- BL:
-
Baseline
- FLS:
-
Fundamentals of Laparoscopic Surgery
- LSS:
-
Laparoscopic surgical skills
- PT:
-
Post-training test
- RT:
-
Retention test
References
McCluney AL, Vassiliou MC, Kaneva PA, Cao J, Stanbridge DD, Feldman LS, Fried GM (2007) FLS simulator performance predicts intraoperative laparoscopic skill. Surg Endosc 21(11):1991–1995. doi:10.1007/s00464-007-9451-1
Scott DJ, Dunnington GL (2008) The new ACS/APDS skills curriculum: moving the learning curve out of the operating room. J Gastrointest Surg 12(2):213–221. doi:10.1007/s11605-007-0357-y
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240(3):518–525. doi:10.1097/01.sla.0000136941.46529.56
Stefanidis D, Korndorffer JR, Markley S, Sierra R, Scott DJ (2006) Proficiency maintenance: impact of ongoing simulator training on laparoscopic skill retention. J Am Coll Surg 202(4):599–603. doi:10.1016/j.jamcollsurg.2005.12.018
Mashaud LB, Castellvi AO, Hollett LA, Hogg DC, Tesfay ST, Scott DJ (2010) Two-year skill retention and certification exam performance after fundamentals of laparoscopic skills training and proficiency maintenance. Surgery 148(2):194–201. doi:10.1016/j.surg.2010.05.012
Castellvi AO, Hollett LA, Minhajuddin A, Hogg DC, Tesfay ST, Scott DJ (2009) Maintaining proficiency after fundamentals of laparoscopic surgery training: a 1-year analysis of skill retention for surgery residents. Surgery 146(2):387–393. doi:10.1016/j.surg.2009.05.009
Ritter EM, Scott DJ (2007) Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov 14(2):107–112. doi:10.1177/1553350607302329
Schreuder HW, van den Berg CB, Hazebroek EJ, Verheijen RH, Schijven MP (2011) Laparoscopic skills training using inexpensive box trainers: which exercises to choose when constructing a validated training course. BJOG 118(13):1576–1584. doi:10.1111/j.1471-0528.2011.03146.x
Stefanidis D, Sierra R, Korndorffer JR, Dunne JB, Markley S, Touchard CL, Scott DJ (2006) Intensive continuing medical education course training on simulators results in proficiency for laparoscopic suturing. Am J Surg 191(1):23–27. doi:10.1016/j.amjsurg.2005.06.046
Korndorffer JR, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201(1):23–29. doi:10.1016/j.jamcollsurg.2005.02.021
Feldman LS, Hagarty SE, Ghitulescu G, Stanbridge D, Fried GM (2004) Relationship between objective assessment of technical skills and subjective in-training evaluations in surgical residents. J Am Coll Surg 198(1):105–110. doi:10.1016/j.jamcollsurg.2003.08.020
Bonrath EM, Weber BK, Fritz M, Mees ST, Wolters HH, Senninger N, Rijcken E (2012) Laparoscopic simulation training: testing for skill acquisition and retention. Surgery 152(1):12–20. doi:10.1016/j.surg.2011.12.036
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199(1):115–120. doi:10.1016/j.amjsurg.2009.07.035
Forbes SS, Fitzgerald PG, Birch DW (2006) Undergraduate surgical training: variations in program objectives and curriculum implementation across Canada. Can J Surg 49(1):46–50
Engum SA (2003) Do you know your students’ basic clinical skills exposure? Am J Surg 186(2):175–181
Derossis AM, Bothwell J, Sigman HH, Fried GM (1998) The effect of practice on performance in a laparoscopic simulator. Surg Endosc 12(9):1117–1120
Rosenthal ME, Ritter EM, Goova MT, Castellvi AO, Tesfay ST, Pimentel EA, Hartzler R, Scott DJ (2010) Proficiency-based Fundamentals of Laparoscopic Surgery skills training results in durable performance improvement and a uniform certification pass rate. Surg Endosc 24(10):2453–2457. doi:10.1007/s00464-010-0985-2
Kimmerle M, Mainwaring L, Borenstein M (2003) The functional repertoire of the hand and its application to assessment. Am J Occup Ther 57(5):489–498
Krumlinde-Sundholm L, Eliasson AC (2002) Comparing tests of tactile sensibility: aspects relevant to testing children with spastic hemiplegia. Dev Med Child Neurol 44(9):604–612
Wanzel KR, Hamstra SJ, Anastakis DJ, Matsumoto ED, Cusimano MD (2002) Effect of visual-spatial ability on learning of spatially-complex surgical skills. Lancet 359(9302):230–231
Wanzel KR, Hamstra SJ, Caminiti MF, Anastakis DJ, Grober ED, Reznick RK (2003) Visual-spatial ability correlates with efficiency of hand motion and successful surgical performance. Surgery 134(5):750–757
Brandt MG, Davies ET (2006) Visual-spatial ability, learning modality and surgical knot tying. Can J Surg 49(6):412–416
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors do not have any commercial and financial connection that can pose a conflict of interest to the findings of this manuscript.
Author contributions
Drs. Sant’Ana and Cavalini contributed to design, data collection, analysis, writing and review of the manuscript. Dr. Negrello helped in data acquisition. Drs. Bonin, Loureiro, Dimbarre and Claus contributed to review of the manuscript. Dr. Salvalaggio helped in design, analysis, writing and review of the manuscript.
Rights and permissions
About this article
Cite this article
Sant’Ana, G.M., Cavalini, W., Negrello, B. et al. Retention of laparoscopic skills in naive medical students who underwent short training. Surg Endosc 31, 937–944 (2017). https://doi.org/10.1007/s00464-016-5063-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5063-y