Abstract
Background
Ultravision™ is a new device that utilizes electrostatic precipitation to clear surgical smoke. The aim was to evaluate its performance during laparoscopic cholecystectomy.
Methods
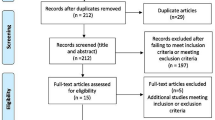
Patients undergoing laparoscopic cholecystectomy were randomized into “active (device on)” or “control (device off).” Three operating surgeons scored the percentage effective visibility and three reviewers scored the percentage of the procedure where smoke was present. All assessors also used a 5-point scale (1 = imperceptible/excellent and 5 = very annoying/bad) to rate visual impairment. Secondary outcomes were the number of smoke-related pauses, camera cleaning, and pneumoperitoneum reductions. Mean results are presented with 95 % confidence intervals (CI).
Results
In 30 patients (active 13, control 17), the effective visibility was 89.2 % (83.3–95.0) for active cases and 71.2 % (65.7–76.7) for controls. The proportion of the procedure where smoke was present was 41.1 % (33.8–48.3) for active cases and 61.5 % (49.0–74.1) for controls. Operating surgeons rated the visual impairment as 2.2 (1.7–2.6) for active cases and 3.2 (2.8–3.5) for controls. Reviewers rated the visual impairment as 2.3 (2.0–2.5) for active cases and 3.2 (2.8–3.7) for controls. In the active group, 23 % of procedures were paused to allow smoke clearance compared to 94 % of control cases. Camera cleaning was not needed in 85 % of active procedures and 35 % of controls. The pneumoperitoneum was reduced in 0 % of active cases and 88 % of controls.
Conclusions
Ultravision™ improves visibility during laparoscopic surgery and reduces delays in surgery for smoke clearance and camera cleaning.










Similar content being viewed by others
References
Spruce L, Braswell ML (2012) Implementing AORN recommended practices for electrosurgery. AORN J 96(3):373–388
British Occupational Hygiene Society (2006) COSHH guidance: surgical smoke. Available at: http://www.bohs.org/uploadedFiles/Groups/Pages/Surgical_smoke.pdf. Accessed 7 Jan 2013
National Institute for Occupation Safety and Health (1996) Control of smoke from laser/electric surgical procedures. Available at: http://www.cdc.gov/niosh/docs/hazardcontrol/pdfs/hc11.pdf. Accessed 7 Jan 2013
CSA Group (2009) Surgical, diagnostic, therapeutic, aesthetic plume scavenging. Available at: http://www.csa.ca/cm/ca/en/home. Accessed 7 Jan 2013
Hollmann R, Hort CE, Kammer E, Naegele M, Sigrist MW, Meuli-Simmen C (2004) Smoke in the operating theatre: an unregarded source of danger. Plast Reconstr Surg 114(2):458–463
Lin YW, Fan SZ, Chang KH, Huang CS, Tang CS (2010) A novel inspection protocol to detect volatile compounds in breast surgery electrocautery smoke. J Formos Med Assoc 109(7):511–516
Moot AR, Ledingham KM, Wilson PF, Senthilmohan ST, Lewis DR, Roake J, Allardyce R (2007) Composition of volatile organic compounds in diathermy plume as detected by selected ion flow tube mass spectrometry. ANZ J Surg 77:20–23
Sawchuk WS, Weber PJ, Lowy DR, Dzubow LM (1989) Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: detection and protection. J Am Acad Dermatol 21:41–49
Capizzi PJ, Clay RP, Battey MJ (1998) Microbiologic activity in laser resurfacing plume debris. Lasers Surg Med 23:172–174
Gatti JE, Bryant CJ, Noone RB, Murphy JB (1992) The mutagenicity of electrocautery smoke. Recon Surg 89(5):781–784
Mowbray N, Ansell J, Warren N, Wall P, Torkington J (2013) Is surgical smoke harmful to theatre staff? A systematic review. Surg Endosc 27(9):3100–3107
Spearman J, Tsavellas G, Nichols P (2007) Current attitudes and practices towards diathermy smoke. Ann R Coll Surg Engl 89(2):162–165
Wu JS, Luttmann DR, Meininger TA, Soper NJ (1997) Production and systemic absorption of toxic byproducts of tissue combustion during laparoscopic surgery. Surg Endosc 11(11):1075–1079
Ott DE (2008) Laparoscopy and adhesion formation, adhesions and laparoscopy. Semin Reprod Med 26(4):322–330
ITU-T (2000) Subjective video quality assessment methods for multimedia applications. Available at: http://www.videoclarity.com/PDF/T-REC-P.910-199909-I!!PDF-E[1].pdf. Accessed 13 Mar 2013
Pillinger SH, Delbridge L, Lewis DR (2003) Randomised clinical trial of suction versus standard clearance of the diathermy plume. Br J Surg 90:1068–1071
Julious SA (2005) Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat 4(4):287–291
Lawrentschuk N, Fleshner NE, Bolton DM (2010) Laparoscopic lens fogging: a review of etiology and methods to maintain a clear visual field. J Endourol 24(6):905–913
Ansell J, Warren N, Sibbons P et al (2012) The Innervision smoke removal device. Available at: http://www.asgbi.org.uk/liverpool2012/pdfs/abs_poster_ pres/Simulation_and_Technology_in_Surgery.pdf. Accessed 6 Mar 2013
Acknowledgments
James Ansell is supported by a Royal College of Surgeons Research Fellowship. Asalus Medical Instruments Ltd. provided the medical equipment required to conduct the trial.
Disclosures
Neil Warren is the inventor of the Ultravision™ instrument but has received no funds for this trial. Pete Wall and Kim Cocks have received consulting fees from Asalus Medical Instruments Ltd. Jared Torkington is a consultant to Asalus Medical Instruments Ltd. James Ansell, Stuart Goddard, David Scott-Coombes, Richard Whiston, and Michael Stechman have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ansell, J., Warren, N., Wall, P. et al. Electrostatic precipitation is a novel way of maintaining visual field clarity during laparoscopic surgery: a prospective double-blind randomized controlled pilot study. Surg Endosc 28, 2057–2065 (2014). https://doi.org/10.1007/s00464-014-3427-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-014-3427-8