Abstract
Background
Computer-based surgical simulators capture a multitude of metrics based on different aspects of performance, such as speed, accuracy, and movement efficiency. However, without rigorous assessment, it may be unclear whether all, some, or none of these metrics actually reflect technical skill, which can compromise educational efforts on these simulators. We assessed the construct validity of individual performance metrics on the LapVR simulator (Immersion Medical, San Jose, CA, USA) and used these data to create task-specific summary metrics.
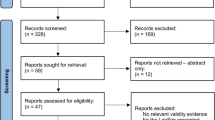
Methods
Medical students with no prior laparoscopic experience (novices, N = 12), junior surgical residents with some laparoscopic experience (intermediates, N = 12), and experienced surgeons (experts, N = 11) all completed three repetitions of four LapVR simulator tasks. The tasks included three basic skills (peg transfer, cutting, clipping) and one procedural skill (adhesiolysis).
Results
We selected 36 individual metrics on the four tasks that assessed six different aspects of performance, including speed, motion path length, respect for tissue, accuracy, task-specific errors, and successful task completion. Four of seven individual metrics assessed for peg transfer, six of ten metrics for cutting, four of nine metrics for clipping, and three of ten metrics for adhesiolysis discriminated between experience levels. Time and motion path length were significant on all four tasks. We used the validated individual metrics to create summary equations for each task, which successfully distinguished between the different experience levels.
Conclusion
Educators should maintain some skepticism when reviewing the plethora of metrics captured by computer-based simulators, as some but not all are valid. We showed the construct validity of a limited number of individual metrics and developed summary metrics for the LapVR. The summary metrics provide a succinct way of assessing skill with a single metric for each task, but require further validation.

Similar content being viewed by others
References
Hawasli A, Featherstone R, Lloyd L, Vorhees M (1996) Laparoscopic training in residency program. J Laparoendosc Surg 6:171–174
Bridges M, Diamond DL (1999) The financial impact of teaching surgical residents in the operating room. Am J Surg 177:28–32
Philibert I, Friedmann P, Williams WT (2002) New requirements for resident duty hours. JAMA 288:1112–1114
Beyer L, Troyer JD, Mancini J, Bladou F, Berdah SV, Karsenty G (2011) Impact of laparoscopy simulator training on the technical skills of future surgeons in the operating room: a prospective study. Am J Surg 202:265–272
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–528
Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150
Park J, MacRae H, Musselman LJ, Rossos P, Hamstra SJ, Wolman S, Reznick RK (2007) Randomized controlled trial of virtual reality simulator training: transfer to live patients. Am J Surg 194:205–211
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463
Sroka G, Feldman LS, Vassiliou MC, Kaneva PA, Fayez R, Fried GM (2010) Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 199:115–120
Derossis AM, Bothwell J, Sigman HH, Fried GM (1998) The effect of practice on performance in a laparoscopic simulator. Surg Endosc 12:1117–1120
Calatayud D, Arora S, Aggarwal R, Kruglikova I, Schulze S, Funch-Jensen P, Grantcharov T (2010) Warm-up in a virtual reality environment improves performance in the operating room. Ann Surg 251:1181–1185
Diesen DL, Erhunmwunsee L, Bennett KM, Ben-David K, Yurcisin B, Ceppa EP, Omotosho PA, Perez A, Pryor A (2011) Effectiveness of laparoscopic computer simulator versus usage of box trainer for endoscopic surgery training of novices. J Surg Educ 68:282–289
Gaba DM (2007) The future vision of simulation in healthcare. Simul Healthc 2:126–135
Satava RM, Gallagher AG, Pellegrini CA (2003) Surgical competence and surgical proficiency: definitions, taxonomy, and metrics. J Am Coll Surg 196:933–937
Downing SM (2003) Validity: on meaningful interpretation of assessment data. Med Educ 37:830–837
Carter FJ, Schijven MP, Aggarwal R, Grantcharov T, Francis NK, Hanna GB, Jakimowicz JJ (2005) Consensus guidelines for validation of virtual reality surgical simulators. Surg Endosc 19:1523–1532
Edelman DA, Mattos MA, Bouwman DL (2010) FLS skill retention (learning) in first year surgery residents. J Surg Res 163:24–28
Sherman V, Feldman LS, Stanbridge D, Kazmi R, Fried GM (2005) Assessing the learning curve for the acquisition of laparoscopic skills on a virtual reality simulator. Surg Endosc 19:678–682
Satava RM, Cuschieri A, Hamdorf J (2003) Metrics for objective assessment. Surg Endosc 17:220–226
Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, Jarvi KA (2004) The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg 240:374–381
Matsumoto ED, Hamstra SJ, Radomski SB, Cusimano MD (2002) The effect of bench model fidelity on endourological skills: a randomized controlled study. J Urol 167:1243–1247
Stefanidis D, Korndorffer JR Jr, Sierra R, Touchard C, Dunne JB, Scott DJ (2005) Skill retention following proficiency-based laparoscopic simulator training. Surgery 138:165–170
Woodrum DT, Andreatta PB, Yellamanchilli RK, Feryus L, Gauger PG, Minter RM (2006) Construct validity of the LapSim laparoscopic surgical simulator. Am J Surg 191:28–32
Eriksen JR, Grantcharov T (2005) Objective assessment of laparoscopic skills using a virtual reality stimulator. Surg Endosc 19:1216–1219
Bell RH (2007) Surgical council on resident education: a new organization devoted to graduate surgical education. J Am Coll Surg 204:341–346
Hamilton EC, Scott DJ, Fleming JB, Rege RV, Laycock R, Bergen PC, Tesfay ST, Jones DB (2002) Comparison of video trainer and virtual reality training systems on acquisition of laparoscopic skills. Surg Endosc 16:406–411
van Dongen KW, Tournoij E, van der Zee DC, Schijven MP, Broeders IA (2007) Construct validity of the LapSim: can the LapSim virtual reality simulator distinguish between novices and experts? Surg Endosc 21:1413–1417
Scott DJ, Ritter EM, Tesfay ST, Pimentel EA, Nagji A, Fried GM (2008) Certification pass rate of 100% for fundamentals of laparoscopic surgery skills after proficiency-based training. Surg Endosc 22:1887–1893
Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM (2005) Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg 241:364–372
American Educational Research Association, American Psychological Association, National Council on Measurement in Education (1999) Standards for educational and psychological testing. American Psychological Association, Washington, DC
Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J (2003) Learning curves and impact of previous operative experience on performance on a virtual reality simulator to test laparoscopic surgical skills. Am J Surg 185:146–149
McDougall EM, Corica FA, Boker JR, Sala LG, Stoliar G, Borin JF, Chu FT, Clayman RV (2006) Construct validity testing of a laparoscopic surgical simulator. J Am Coll Surg 202:779–787
Iwata N, Fujiwara M, Kodera Y, Tanaka C, Ohashi N, Nakayama G, Koike M, Nakao A (2011) Construct validity of the LapVR virtual-reality surgical simulator. Surg Endosc 25:423–428
Derossis AM, Fried GM, Abrahamowicz M, Sigman HH, Barkun JS, Meakins JL (1998) Development of a model for training and evaluation of laparoscopic skills. Am J Surg 175:482–487
Stefanidis D, Scott DJ, Korndorffer JR Jr (2009) Do metrics matter? Time versus motion tracking for performance assessment of proficiency-based laparoscopic skills training. Simul Healthc 4:104–108
Gauger PG, Hauge LS, Andreatta PB, Hamstra SJ, Hillard ML, Arble EP, Kasten SJ, Mullan PB, Cederna PS, Minter RM (2010) Laparoscopic simulation training with proficiency targets improves practice and performance of novice surgeons. Am J Surg 199:72–80
Aggarwal R, Ward J, Balasundaram I, Sains P, Athanasiou T, Darzi A (2007) Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 246:771–779
Gallagher AG, Lederman AB, McGlade K, Satava RM, Smith CD (2004) Discriminative validity of the Minimally Invasive Surgical Trainer in Virtual Reality (MIST-VR) using criteria levels based on expert performance. Surg Endosc 18:660–665
Disclosure
Justin Rivard, Ashley Vergis, Bertram Unger, Krista Hardy, Chris Andrew, Lawrence Gillman, and Jason Park have no conflicts of interest or financial ties to disclose. Funding was received from the Canadian Association of General Surgeons Research Fund by Ethicon Endosurgery.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rivard, J.D., Vergis, A.S., Unger, B.J. et al. Construct validity of individual and summary performance metrics associated with a computer-based laparoscopic simulator. Surg Endosc 28, 1921–1928 (2014). https://doi.org/10.1007/s00464-013-3414-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3414-5