Abstract
Background
Laparoscopic liver resection has not been widely used because of intraoperative bleeding. This problem should be solved with instruments and techniques that require a short learning curve.
Materials and methods
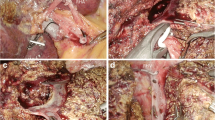
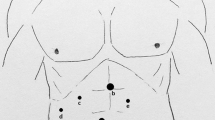
The aim of this work was to present the technique used in our center to perform laparoscopic liver resection using the ‘curettage and aspiration’ technique with laparoscopic Peng’s multifunctional operational dissectors and regional occlusion of inflow and outflow. We retrospectively analyzed patients who underwent a laparoscopic liver resection from August 1998 to August 2012, and collected the conversion rate, operating time, blood loss, hospitalization, bile leakage rate, bleeding rate, and other complications on a yearly basis and in total. We used SPSS software to analyze whether there was a significant difference, and summarized the learning curve of laparoscopic liver resection with various procedures.
Results
We performed 365 cases of laparoscopic liver resection, including left hemihepatectomy, left lateral lobectomy, segmental hepatectomy, non-anatomic liver resection, right hemihepatectomy, and caudate lobectomy. The diseases included liver cancer, hepatolithiasis, liver hemangioma, focal nodular hyperplasia, liver abscess, and metastatic hepatic carcinoma. In total, 63 cases (17.20 %) were converted to open surgery because of severe adhesions, bleeding, or anatomical limitation. Mean blood loss was 370.6 ± 404.0 ml; mean operating time was 150.8 ± 73.0 min; and mean postoperation hospitalization was 9.2 ± 5.3 days. There were four cases (1.32 %) with the complication of bile leakage and two cases of hemorrhage (0.66 %). No intraoperative or postoperative deaths occurred. After finishing 15–30, 43, 35, and 28 cases of laparoscopic left hemihepatectomy, left lateral hepatectomy, non-anatomic liver resection, and segmentectomy, respectively, the average operating time, blood loss, and hospitalization were almost the same as the overall mean results.
Conclusion
The technique used in our center is a safe, fast, and effective approach to laparoscopic liver resection. Our 14 years of experience demonstrates that this technique can prevent postoperative bleeding and bile leakage. A surgeon can master the skill of laparoscopic left hemihepatectomy, left lateral hepatectomy, non-anatomic liver resection, and segmentectomy after ∼15–30, 43, 35, and 28 case procedures, respectively.
Article PDF
Similar content being viewed by others
Avoid common mistakes on your manuscript.
References
Robles R, Marín C, Abellán B, López-Conesa A, Ramírez P, Parrilla P (2006) Right hepatectomy and left hepatectomy performed via hand-assisted laparoscopic surgery. Description of an original technique (in Spanish). Cir Esp 80:326–330
Liu R, Huang ZQ, Zhou NX, Huang XQ, Wang YH, Jiang K, Xiang X (2004) Operational line of laparoscopic liver resections. Zhonghua Yi Xue Za Zhi 84:219–221
Machado MA, Surjan RC, Makdissi FF (2011) Intrahepatic glissonian approach for pure laparoscopic right hemihepatectomy. Surg Endosc 25:3930–3933
Nguyen KT, Gamblin TC, Geller DA (2009) World review of laparoscopic liver resection: 2,804 patients. Ann Surg 250: 831–841
Cai XJ, Yu H, Liang X, Wang YF, Zheng XY, Huang DY, Peng SY (2006) Laparoscopic hepatectomy by curettage and aspiration: experiences of 62 cases. Surg Endosc 20:1531–1535
Peng SY (1994) Multifunctional operational dissectors. China Patent CN1080512
Peng SY, Su Y, Cai XJ (2007) Operational dissectors. China Patent CN3671884
Cai XJ, Gu XJ, Wang YF, Yu H, Liang X (2007) Experience in laparoscopic cholecystectomy by exposing common hepatic duct using blunt dissection to prevent bile duct injury. Zhonghua Yi Xue Za Zhi 87:1425–1426
Peng SY, Li JT, Mou YP, Liu YB, Wu YL, Fang HQ, Cao LP, Chen L, Cai XJ, Peng CH (2003) Different approaches to caudate lobectomy with “curettage and aspiration” technique using a special instrument PMOD: a report of 76 cases. World J Gastroenterol 9:2169–2173
Cai XJ, Wang YF, Liang YL, Yu H, Liang X (2009) Laparoscopic left hemihepatectomy: a safety and feasibility study of 19 cases. Surg Endosc 23:2556–2562
Disclosures
Xiujun Cai, Zheyong Li, Yale Zhang, Hong Yu, Xiao Liang, Renan Jin, and Feng Luo have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (WMV 286650 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Cai, X., Li, Z., Zhang, Y. et al. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc 28, 1334–1341 (2014). https://doi.org/10.1007/s00464-013-3333-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3333-5