Abstract
Objective
To explore the feasibilities between operational approaches for laparoscopic complete mesocolic excision (CME) to right hemicolon cancer.
Methods
This prospective randomized controlled trial included patients admitted to a Shanghai minimally invasive surgical center to receive laparoscopic CME from September 2011 to January 2013 randomized into two groups: hybrid medial approach (HMA) and completely medial approach (CMA). The feasibilities and strategies of the two techniques were studied and compared. Furthermore, the operation time and vessel-related complications were designed to be the primary end points, and other operational findings, including the classification of the surgical plane and postoperative recovery, were designed to be the secondary end points for this study.
Results
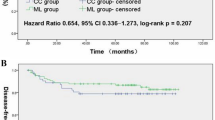
After screening, 50 cases were allocated to the HMA group and 49 to the CMA group. Within the HMA group, there were 48 cases graded with mesocolic plane and 2 with intramesocolic plane. For the CMA group, there were 42 cases graded with mesocolic plane and seven with intramesocolic plane. The differences between the two were insignificant, as were the number of lymph nodes retrieved. The mean±standard deviation total operation time for the CMA group was 128.3 ± 36.4 min, which was significantly shorter than that for the HMA group, 142.6 ± 34.8 min. For the CMA group, the time involved in central vessel ligations and laparoscopic procedures was 58.5 %, 14.1 and 81.2 ± 23.5 min, respectively, which were shorter than the HMA group. The vessel-related complication rate was significantly higher in the HMA group.
Conclusions
Laparoscopic CME via the total medial approach is technically feasible after the precise identification of the surgical planes and spaces for the right hemicolon. The procedure has a shorter operation time and fewer vessel-related complications.



Similar content being viewed by others
References
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis 11:354–364
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28:272–278
Eiholm S, Ovesen H (2010) Total mesocolic excision versus traditional resection in right-sided colon cancer—method and increased lymph node harvest. Dan Med Bull 57:A4224
Pramateftakis MG (2010) Optimizing colonic cancer surgery: high ligation and complete mesocolic excision during right hemicolectomy. Tech Coloproctol 14(Suppl 1):S49–S51
Zheng MH, Feng B, Lu AG, Li JW, Wang ML, Mao ZH, Hu YY, Dong F, Hu WG, Li DH, Zang L, Peng YF, Yu BM (2005) Laparoscopic versus open right hemicolectomy with curative intent for colon carcinoma. World J Gastroenterol 11:323–326
Feng B, Sun J, Ling TL, Lu AG, Wang ML, Chen XY, Ma JJ, Li JW, Zang L, Han DP, Zheng MH (2012) Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc 26:3669–3675
Adamina M, Manwaring ML, Park KJ, Delaney CP (2012) Laparoscopic complete mesocolic excision for right colon cancer. Surg Endosc 26:2976–2980
Zhang C, Ding ZH, Yu HT, Yu J, Wang YN, Hu YF, Li GX (2011) Retrocolic spaces: anatomy of the surgical planes in laparoscopic right hemicolectomy for cancer. Am Surg 77:1546–1552
West NP, Morris EJ, Rotimi O, Cairns A, Finan PJ, Quirke P (2008) Pathology grading of colon cancer surgical resection and its association with survival: a retrospective observational study. Lancet Oncol 9:857–865
Japanese Society for Cancer of the Colon and Rectum (2009) Japanese classification of colorectal carcinoma, 2nd edn. Kanehara, Tokyo
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30:1763–1769
Acknowledgments
We gratefully acknowledge the National High Technology Research and Development Program of China (863 Program), the Science and Technology Commission of Shanghai Municipality, and the Shenkang Center of Hospital Development for financial support (2012AA021103, 1141195070, 11411950701, SHDC12010116). In addition, we appreciate the contributions of their coworkers and friends to this study, as well as the editors and reviewers for their input.
Disclosures
Bo Feng, Tian-Long Ling, Ai-Guo Lu, Ming-Liang Wang, Jun–Jun Ma, Jian-Wen Li, Lu Zang, Jing Sun, and Min-Hua Zheng have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Feng, B., Ling, TL., Lu, AG. et al. Completely medial versus hybrid medial approach for laparoscopic complete mesocolic excision in right hemicolon cancer. Surg Endosc 28, 477–483 (2014). https://doi.org/10.1007/s00464-013-3225-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3225-8