Abstract
Background
Thoracoscopic esophagectomy is a feasible technique that has been shown to be safe for the treatment of esophageal cancer. There continues to be controversy about the optimal position during thoracoscopic esophagectomy. In this study, we compared the intraoperative hemodynamic parameters, clinical pathological characteristics, as well as postoperative complications in patients who underwent thoracoscopic esophagectomy in the prone position (PP) or left-lateral decubitus position (LDP).
Methods
Between January 2011 and June 2011, 23 patients underwent thoracoscopic esophagectomies for cancer of the esophagus in LDP (group A). Since February 2011, we have performed thoracoscopic esophagectomies for cancer of the esophagus in PP for 21 patients (group B). The demographics and clinicopathologic factors, as well as the intraoperative hemodynamic parameters, of the two groups were analyzed.
Results
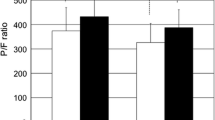
No postoperative death occurred in these 44 patients. Overall morbidity was similar in the two groups. No significant difference in the length of operation or number of retrieved mediastinal nodes between the two groups was observed, but the intraoperative blood loss in group A was significantly higher than in group B (P = 0.0228). There was no significant difference of the intraoperative mean arterial pressure, central venous pressure, heart rate, and stroke volume variation between the two groups and various positions. In group A, the cardiac output (CO), cardiac index (CI), as well as stroke volume index (SVI) did not exhibit significant difference after altering patients’ position from LDP to SP. However, patients who underwent thorascopic esophagectomy in PP had lower CO, CI, and SVI than in LDP during the thoracoscopic stage.
Conclusions
Compared with the PP, the LDP could provide more excellent hemodynamic parameters during thoracoscopic esophagectomy. However, the various hemodynamic statuses did not exert significant influence on the occurrence of postoperative complications.

Similar content being viewed by others
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ (2008) Cancer statistics, 2008. CA Cancer J Clin 58:71–96
Enzinger PC, Mayer RJ (2003) Esophageal cancer. N Engl J Med 349:2241–2252
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37:7–11
Law S, Fok M, Chu KM, Wong J (1997) Thoracoscopic esophagectomy for esophageal cancer. Surgery 122:8–14
Taguchi S, Osugi H, Higashino M, Tokuhara T, Takada N, Takemura M, Lee S, Kinoshita H (2003) Comparison of three-field esophagectomy for esophageal cancer incorporating open or thoracoscopic thoracotomy. Surg Endosc 17:1445–1450
Fukunaga T, Kidokoro A, Fukunaga M, Nagakari K, Suda M, Yoshikawa S (2001) Kinetics of cytokines and PMN-E in thoracoscopic esophagectomy. Surg Endosc 15:1484–1487
Osugi H, Takemura M, Higashino M, Takada N, Lee S, Kinoshita H (2003) A comparison of video-assisted thoracoscopic oesophagectomy and radical lymph node dissection for squamous cell cancer of the oesophagus with open operation. Br J Surg 90:108–113
Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position: experience of 130 patients. J Am Coll Surg 203:7–16
Jarral OA, Purkayastha S, Athanasiou T, Zacharakis E (2011) Should thoracoscopic three-stage esophagectomy be performed in the prone or left lateral decubitus position? Interact Cardiovasc Thorac Surg 13:60–65
Guo W, Zhao YP, Jiang YG, Niu HJ, Liu XH, Ma Z, Wang RW (2012) Prevention of postoperative chylothorax with thoracic duct ligation during video-assisted thoracoscopic esophagectomy for cancer. Surg Endosc 26:1332–1336
Luketich JD, Alvelo-Rivera M, Buenaventura PO, Christie NA, McCaughan JS, Litle VR, Schauer PR, Close JM, Fernando HC (2003) Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 238:486–494
Luketich JD, Schauer PR, Christie NA, Weigel TL, Raja S, Fernando HC, Keenan RJ, Nguyen NT (2000) Minimally invasive esophagectomy. Ann Thorac Surg 70:906–911
Luketich JD, Pennathur A, Awais O, Levy RM, Keeley S, Shende M, Christie NA, Weksler B, Landreneau RJ, Abbas G, Schuchert MJ, Nason KS (2012) Outcomes after minimally invasive esophagectomy: review of over 1,000 patients. Ann Surg 256:95–103
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Butler N, Collins S, Memon B, Memon MA (2011) Minimally invasive oesophagectomy: current status and future direction. Surg Endosc 25:2071–2083
Watson DI, Davies N, Jamieson GG (1999) Totally endoscopic Ivor Lewis esophagectomy. Surg Endosc 13:293–297
Fabian T, McKelvey AA, Kent MS, Federico JA (2007) Prone thoracoscopic esophageal mobilization for minimally invasive esophagectomy. Surg Endosc 21:1667–1670
Puntambekar SP, Agarwal GA, Joshi SN, Rayate NV, Sathe RM, Patil AM (2010) Thoracolaparoscopy in the lateral position for esophageal cancer: the experience of a single institution with 112 consecutive patients. Surg Endosc 24:2407–2414
Edgcombe H, Carter K, Yarrow S (2008) Anaesthesia in the prone position. Br J Anaesth 100:165–183
Dharmavaram S, Jellish WS, Nockels RP, Shea J, Mehmood R, Ghanayem A, Kleinman B, Jacobs W (2006) Effect of prone positioning systems on hemodynamic and cardiac function during lumbar spine surgery: an echocardiographic study. Spine (Phila Pa 1976) 31:1388–1393
Yokoyama M, Ueda W, Hirakawa M, Yamamoto H (1991) Hemodynamic effect of the prone position during anesthesia. Acta Anaesthesiol Scand 35:741–744
Acknowledgment
Disclosures
Drs. Ying-Bo Zou, Hong Yan, Xue-Hai Liu, Yin-Jie Zhao, Yao-Guang Jiang, Ru-Wen Wang, and Wei Guo have no conflict of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ying-Bo Zou and Hong Yan contributed equally to this study.
Rights and permissions
About this article
Cite this article
Zou, YB., Yan, H., Liu, XH. et al. Lateral position could provide more excellent hemodynamic parameters during video-assisted thoracoscopic esophagectomy for cancer. Surg Endosc 27, 3720–3725 (2013). https://doi.org/10.1007/s00464-013-2953-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2953-0