Abstract
Background
The potential effects of laparoscopic surgery on intra- and postoperative intraocular pressure (IOP) are not completely understood. Although prior studies have reported that pneumoperitoneum may increase IOP, it is not clear whether this increase is related to the effects of pneumoperitoneum or to the patient’s position, such as the Trendelenburg position. This study aimed to evaluate the potential fluctuations of IOP during colorectal laparoscopic surgery in two groups of patients: those with and those without Trendelenburg positioning.
Methods
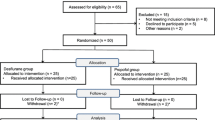
For this prospective study 45- to 85-year-old patients undergoing laparoscopic colorectal surgery were enrolled after a thorough ophthalmologic assessment. The study protocol included measurement of IOP at eight different time points (before, during, and after surgery) using a contact tonometer in both eyes.
Results
The study enrolled 29 patients: 17 (58.6 %) with Trendelenburg position placement during surgery and 12 (41.4 %) without Trendelenburg positioning. The two groups did not differ in terms of gender, age, body mass index (BMI), American Society of Anesthesiology (ASA) class, or operative time. In all the patients, pneumoperitoneum induction led to a mild rise in IOP, averaging 4.1 mmHg. The patients with Trendelenburg positioning showed a greater increase than the patients without it (5.05 vs 4.23 mmHg at 45 min; p = 0.179), but IOP evaluation 48 h after surgery showed no substantial differences between the two groups. Among the 29 patients, 17 (58.6 %) showed an increase in IOP of 5 mmHg or more during surgery. A greater percentage of the patients who underwent Trendelenburg positioning showed an IOP increase of 5 mmHg or more (76.5 vs 33.3 %; p = 0.020). At the multivariate analysis, no potential predictors of increased IOP during surgery was identified.
Conclusions
Standard pneumoperitoneum (≤14 mmHg) led to mild and reversible IOP increases. A trend was observed toward a greater IOP increase in patients with Trendelenburg positioning. Thus, the patient’s position during surgery may represent a stronger risk factor for IOP increase than pneumoperitoneum-related intraabdominal pressure.

Similar content being viewed by others
References
Yanagi M, Kawasaki R, Wang JJ, Wong TY, Crowston J, Kiuchi Y (2011) Vascular risk factors in glaucoma: a review. Clin Exp Ophthalmol 39:252–258
Sung KR, Cho JW, Lee S, Yun SC, Choi J, Na JH, Lee Y, Kook MS (2011) Characteristics of visual field progression in medically treated normal-tension glaucoma patients with unstable ocular perfusion pressure. Invest Ophthalmol Vis Sci 52:737–743
Medeiros FA, Weinreb RN, Zangwill LM, Alencar LM, Sample PA, Vasile C, Bowd C (2008) Long-term intraocular pressure fluctuations and risk of conversion from ocular hypertension to glaucoma. Ophthalmology 115:934–940
Law SK, Nguyen AM, Coleman AL, Caprioli J (2007) Severe loss of central vision in patients with advanced glaucoma undergoing trabeculectomy. Arch Ophthalmol 125:1044–1050
Ma Y, Yang Z, Qin H, Wang Y (2011) A meta-analysis of laparoscopy compared with open colorectal resection for colorectal cancer. Med Oncol 28:925–933
Lourenco T, Murray A, Grant A, McKinley A, Krukowski Z, Vale L (2008) Laparoscopic surgery for colorectal cancer: safe and effective? a systematic review. Surg Endosc 22:1146–1160
Mowafi HA, Al-Ghamdi A, Rushood A (2003) Intraocular pressure changes during laparoscopy in patients anesthetized with propofol total intravenous anesthesia versus isoflurane inhaled anesthesia. Anesth Analg 97:471–474
Awad H, Santilli S, Ohr M, Roth A, Yan W, Fernandez S, Roth S, Patel V (2009) The effects of steep Trendelenburg positioning on intraocular pressure during robotic radical prostatectomy. Anesth Analg 109:473–478
Lentschener C, Leveque JP, Mazoit JX, Benhamou D (1998) The effect of pneumoperitoneum on intraocular pressure in rabbits with alpha-chymotrypsin-induced glaucoma. Anesth Analg 86:1283–1288
Sit AJ (2009) Continuous monitoring of intraocular pressure: rationale and progress toward a clinical device. J Glaucoma 18:272–279
Scuderi GL, Cascone NC, Regine F, Perdicchi A, Cerulli A, Recupero SM (2011) Validity and limits of the rebound tonometer (ICare®): clinical study. Eur J Ophthalmol 21:251–257
Brusini P, Salvetat ML, Zeppieri M, Tosoni C, Parisi L (2006) Comparison of ICare tonometer with Goldmann applanation tonometer in glaucoma patients. J Glaucoma 15:213–217
Tarek Shaarawy T, Sherwood MB, Hitchings RA, Crowston JG (2009) Glaucoma. Saunders Ltd, Philadelphia, PA
Morino M, Parini U, Girando G, Salval M, Brachet Contul R, Garrone C (2003) Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg 237:335–342
Hosmer DW, Lemeshow S (2000) Applied logistic regression (Wiley Series in probability and statistics), 2nd edn. Wiley, New York, NY
Sultan MB, Mansberger SL, Lee PP (2009) Understanding the importance of IOP variables in glaucoma: a systematic review. Surv Ophthalmol 54:643–662
Abraham LM, Epasinghe NC, Selva D, Casson R (2008) Comparison of the ICare rebound tonometer with the Goldmann applanation tonometer by experienced and inexperienced tonometrists. Eye Lond 22:503–506
Pinkney TD, King AJ, Walter C, Wilson TR, Maxwell-Armstrong C, Acheson AG (2012) Raised intraocular pressure (IOP) and perioperative visual loss in laparoscopic colorectal surgery: a catastrophe waiting to happen? A systematic review of evidence from other surgical specialities. Tech Coloproctol 16:331–335
Shen Y, Drum M, Roth S (2009) The prevalence of perioperative visual loss in the United States: a 10-year study from 1996 to 2005 of spinal, orthopedic, cardiac, and general surgery. Anesth Analg 109:1534–1545
Liu JH, Sit AJ, Weinreb RN (2005) Variation of 24-hour intraocular pressure in healthy individuals: right eye versus left eye. Ophthalmology 112:1670–1675
Acknowledgments
The authors thank Prof. Jonathan G. Crowston, Head of the Department of Ophthalmology at the University of Melbourne, for his help in reviewing the manuscript.
Disclosures
Andrea Grosso, Gitana Scozzari, Fabrizio Bert, Maria Antonietta Mabilia, Roberta Siliquini, and Mario Morino have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grosso, A., Scozzari, G., Bert, F. et al. Intraocular pressure variation during colorectal laparoscopic surgery: standard pneumoperitoneum leads to reversible elevation in intraocular pressure. Surg Endosc 27, 3370–3376 (2013). https://doi.org/10.1007/s00464-013-2919-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2919-2