Abstract
Background
The aim of this study was to determine growth in trainee laparoscopic skill as recorded by the TrEndo laparoscopic simulator during a laparoscopic training course, compared to an expert level.
Methods
A prospective observational cohort study was conducted between February 1 and November 31, 2010. Trainees in laparoscopic surgery completed a basic laparoscopic suturing task on a laparoscopic box trainer at three successive assessment points during a laparoscopic training course. Experts were assessed only once to define an expert level. The TrEndo recorded four motion analysis parameters (MAPs) individually for each hand and the amount of time taken to complete the suturing task.
Results
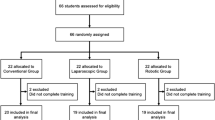
Seventy-two residents and 56 experts were included in this study. Overall, the amount of time taken on the suturing task and seven out of eight MAPs significantly increased toward an expert level during the course, representing an improvement in task efficiency. During the first training day, the amount of time spent on the suturing task and five out of eight MAPs improved significantly. After the retention period, five out of eight MAPS demonstrated a significant improvement compared to the end of the first training day.
Conclusions
Laparoscopic skill of trainees as recorded by the TrEndo laparoscopic simulator grows toward an expert level during a laparoscopic training course in a large and heterogeneous study group. Construct validity of the TrEndo is established.


Similar content being viewed by others
References
van Empel P, van der Veer W, van Rijssen L, Cuesta M, Scheele F, Bonjer H, Meijerink W (2012) Mapping the maze of minimally invasive surgery simulators. J Laparoendosc Adv Surg Tech A 22:51–60
Fried GM, Feldman LS, Vassiliou MC, Fraser SA, Stanbridge D, Ghitulescu G, Andrew CG (2004) Proving the value of simulation in laparoscopic surgery. Ann Surg 240:518–525
Scott DJ, Bergen PC, Rege RV, Laycock R, Tesfay ST, Valentine RJ, Euhus DM, Jeyarajah DR, Thompson WM, Jones DB (2000) Laparoscopic training on bench models: better and more cost effective than operating room experience? J Am Coll Surg 191:272–283
Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463
Goova MT, Hollett LA, Tesfay ST, Gala RB, Puzziferri N, Kehdy FJ, Scott DJ (2008) Implementation, construct validity, and benefit of a proficiency-based knot-tying and suturing curriculum. J Surg Educ 65:309–315
Scott DJ, Ritter EM, Tesfay ST, Pimentel EA, Nagji A, Fried GM (2008) Certification pass rate of 100 % for fundamentals of laparoscopic surgery skills after proficiency-based training. Surg Endosc 22:1887–1893
Botden SMBI, Jakimowicz JJ (2009) What is going on in augmented reality simulation in laparoscopic surgery? Surg Endosc 23:1693–1700
Aggarwal R, Hance J, Undre S, Ratnasothy J, Moorthy K, Chang A, Darzi A (2006) Training junior operative residents in laparoscopic suturing skills is feasible and efficacious. Surgery 139:729–734
Andreatta PB, Woodrum DT, Birkmeyer JD, Yellamanchilli RK, Doherty GM, Gauger PG, Minter RM (2006) Laparoscopic skills are improved with LapMentor training: results of a randomized, double-blinded study. Ann Surg 243:854–860
Lentz GM, Mandel LS, Lee D, Gardella C, Melville J, Goff BA (2001) Testing surgical skills of obstetric and gynecologic residents in a bench laboratory setting: validity and reliability. Am J Obstet Gynecol 184:1462–1468
Grober ED, Hamstra SJ, Wanzel KR, Reznick RK, Matsumoto ED, Sidhu RS, Jarvi KA (2004) The educational impact of bench model fidelity on the acquisition of technical skill: the use of clinically relevant outcome measures. Ann Surg 240:374–381
Chmarra MK, Grimbergen CA, Dankelman J (2007) Systems for tracking minimally invasive surgical instruments. Minim Invasive Ther Allied Technol 16:328–340
Chmarra MK, Bakker NH, Grimbergen CA, Dankelman J (2006) TrEndo, a device for tracking minimally invasive surgical instruments in training setups. Sens Actuators A Phys 126:328–334
van Empel PJ, van Rijssen LB, Commandeur JP, Verdam MGE, Huirne JA, Scheele F, Bonjer HJ, Meijerink WJ (2012) Validation of a new box trainer-related tracking device: the TrEndo. Surg Endosc 26:2346–2352
Smith SGT, Torkington J, Brown TJ, Taffinder NJ, Darzi A (2002) Motion analysis. Surg Endosc 16:640–645
Madan AK, Frantzides CT, Shervin N, Tebbit CL (2003) Assessment of individual hand performance in box trainers compared to virtual reality trainers. Am Surg 69:1112–1114
Van Sickle KR, McClusky DA, Gallagher AG, Smith CD (2005) Construct validation of the ProMIS simulator using a novel laparoscopic suturing task. Surg Endosc 19:1227–1231
Vossen C, Van Ballaer P, Shaw RW, Koninckx PR (1997) Effect of training on endoscopic intracorporeal knot tying. Hum Reprod 12:2658–2663
Munz Y, Almoudaris AM, Moorthy K, Dosis A, Liddle AD, Darzi AW (2007) Curriculum-based solo virtual reality training for laparoscopic intracorporeal knot tying: objective assessment of the transfer of skill from virtual reality to reality. Am J Surg 193:774–783
Aggarwal R, Grantcharov T, Moorthy K, Milland T, Papasavas P, Dosis A, Bello F, Darzi A (2007) An evaluation of the feasibility, validity, and reliability of laparoscopic skills assessment in the operating room. Ann Surg 245:992
Moorthy K, Munz Y, Dosis A, Bello F, Chang A, Darzi A (2004) Bimodal assessment of laparoscopic suturing skills. Surg Endosc 18:1608–1612
Stefanidis D, Haluck R, Pham T, Dunne JB, Reinke T, Markley S, Korndorffer JR, Arellano P, Jones DB, Scott DJ (2007) Construct and face validity and task workload for laparoscopic camera navigation: virtual reality versus videotrainer systems at the SAGES learning center. Surg Endosc 21:1158–1164
VU University Medical Center (2007) Advanced suturing course, 2007–2012. http://www.vumc.nl/afdelingen/PAOG/Laparoscopiecursus/
Furnee EJB, van Empel PJ, Delavary BM, van der Peet DL, Cuesta MA, Meijerink WJHJ (2009) Evaluation of a technical skills training program in surgical residents. J Laparoendosc Adv Surg Tech A 19:615–621
van Empel PJ, Verdam MGE, Strypet M, van Rijssen LB, Huirne JA, Scheele F, Bonjer HJ, Meijerink WJ (2012) Voluntary autonomous simulator based training in minimally invasive surgery, residents’ compliance and reflection. J Surg Educ 69:564–570
Chmarra MK, Klein S, de Winter JCF, Jansen FW, Dankelman J (2010) Objective classification of residents based on their psychomotor laparoscopic skills. Surg Endosc 24:1031–1039
Rosser JC, Rosser LE, Savalgi RS (1997) Skill acquisition and assessment for laparoscopic surgery. Arch Surg 132:200–204
Yamaguchi S, Yoshida D, Kenmotsu H, Yasunaga T, Konishi K, Ieiri S, Nakashima H, Tanoue K, Hashizume M (2011) Objective assessment of laparoscopic suturing skills using a motion-tracking system. Surg Endosc 25:771–775
Stefanidis D, Acker CE, Greene FL (2010) Performance goals on simulators boost resident motivation and skills laboratory attendance. J Surg Educ 67:66–70
Crofts JF, Bartlett C, Ellis D, Hunt LP, Fox R, Draycott TJ (2007) Management of shoulder dystocia: skill retention 6 and 12 months after training. Obstet Gynecol 110:1069–1074
Verdaasdonk EGG, Dankelman J, Schijven MP, Lange JF, Wentink M, Stassen LPS (2009) Serious gaming and voluntary laparoscopic skills training: a multicenter study. Minim Invasive Ther Allied Technol 18:232–238
Hardyck C, Petrinovich LF (1977) Left-handedness. Psychol Bull 84:385–404
Roberts KE, Bell RL, Duffy AJ (2006) Evolution of surgical skills training. World J Gastroenterol 12:3219–3224
Ritchie WPJ (2004) Basic certification in surgery by the American board of surgery (ABS): what does it mean? Does it have value? Is it relevant? A personal opinion. Ann Surg 239:133–139
Ghaderi I, Vaillancourt M, Sroka G, Kaneva PA, Seagull FJ, George I, Sutton E, Park AE, Vassiliou MC, Fried GM, Feldman LS (2011) Performance of simulated laparoscopic incisional hernia repair correlates with operating room performance. Am J Surg 201:40–45
Cotin S, Stylopoulos N, Ottensmeyer M, Neumann P, Rattner D, Dawson S (2002) Metrics for laparoscopic skills trainers: the weakest link! Med Image Comput Comput Assist Intervent 2002:35–43
Dankelman J, Chmarra MK, Verdaasdonk EGG, Stassen LPS, Grimbergen CA (2005) Fundamental aspects of learning minimally invasive surgical skills. Minim Invasive Ther Allied Technol 14:247–256
Acknowledgments
The authors thank Dr. J. J. van den Dobbelsteen, Department of BioMechanical Engineering, Delft University of Technology, for his contribution and technical support regarding the TrEndo tracking device. We want to thank R. P. M. de Hoon, Department of Surgery, VU University Medical Center, for his very important contributions to the organization and logistics of the advanced suturing training program.
Disclosures
Pieter J. van Empel, Joris P. Commandeur, Lennart B. van Rijssen, Mathilde G. E. Verdam, Judith Huirne, Fedde Scheele, H. Jaap Bonjer, and Wilhelmus J. Meijerink have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Empel, P.J., Commandeur, J.P., van Rijssen, L.B. et al. Learning curve on the TrEndo laparoscopic simulator compared to an expert level. Surg Endosc 27, 2934–2939 (2013). https://doi.org/10.1007/s00464-013-2859-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-2859-x